Practice - Texas Board of Nursing Position Statements
15.1 Nurses Carrying out Orders from Physician Assistants
|
|
The purpose of this position statement is to provide guidance to nurses with regard to carrying out orders from Physician Assistants (PAs).
The Nursing Practice Act (NPA) includes the "administration of medications or treatments ordered by a physician, podiatrist or dentist" as part of the practice of nursing.1,2 There are no other healthcare professionals listed thus leading to questions regarding nurses carrying out orders from other licensed healthcare providers. Although PAs are not included in the NPA, the Board recognizes that nurses work collaboratively with PAs to provide patient care in various practice settings.
The PA is licensed and regulated by the Texas Physician Assistant Board.3 PAs may provide medical aspects of care, including ordering or prescribing medications and treatments, as delegated by a physician consistent with laws, rules and regulations applicable to the PAs’ practice including those of the Texas Medical Board (TMB) Chapter 193.4 A physician is not required to be present at all times at the location where the PA is providing care and orders are not required to be countersigned by the physician. A nurse may carry out these orders. As with any order, the nurse must seek clarification if he/she believes the order or treatment is inaccurate, non-efficacious or contraindicated by consulting with the PA and physician as appropriate.5 A list of physician assistants credentialed by the medical staff and policies directing their practice should be available to the nursing staff.
References
1 Nursing Practice Act, TOC §301.002(2)
2 Texas Board of Nursing (2017). Position statement 15.25, Administration of Medication & Treatments by LVNs.
3 Physician Assistant Licensing Act, TOC Chapter 204 and 22 TAC Chapter 185
4 22 TAC §§185.2(17); 185.10, 193.2(17) & 193.2(18)
5 22 TAC §217.11(1)(N)
(Board Action: 01/1994; Revised: 01/2005; 01/2006; 01/2010; 01/2012; 01/2016; 01/2017; 01/2018)
(Reviewed: 01/2007; 01/2008; 01/2009; 01/2011; 01/2013; 01/2014; 01/2015; 01/2019 ;01/2020; 01/2021)
Return to top
|
15.2 The Role of the Licensed Vocational Nurse in the Pronouncement of Death
|
|
Licensed vocational nurses (LVNs) do not have the authority to legally determine death, diagnose death, or otherwise pronounce death in the State of Texas. Regardless of practice setting, the importance of initiating cardiopulmonary resuscitation (CPR) in cases where no clear do-not-resuscitate (DNR) orders exist is imperative. The Board of Nursing (BON) has investigated cases involving the failure of a LVN to initiate CPR in the absence of a DNR order. Position Statement 15.20, Registered Nurses in the Management of an Unwitnessed Arrest in a Resident in a Long Term Care Facility, has additional information in regards to initiating CPR.
It is within the LVN scope of practice as defined by 22 TAC §217.11(1)-(2) (effective 9/28/2004) and Position Statement 15.27, The Licensed Vocational Nurse Scope of Practice, for a LVN to gather data and perform a focused assessment regarding a patient, to recognize significant changes in a patient’s condition, and to report said data and observation of significant changes to the physician. The LVN’s focused assessment should include nursing observations to determine the presence or absence of the following presumptive or conclusive signs of death:
Presumptive Signs of Death
- The patient is unresponsive,
- The patient has no respirations,
- The patient has no pulse,
- The patient’s pupils are fixed and dilated,
- The patient’s body temperature indicates hypothermia: skin is cold relative to the patient’s baseline skin temperature,
- The patient has generalized cyanosis, and
Conclusive Signs of Death
- There is presence of livor mortis (venous pooling of blood in dependent body parts causing purple discoloration of the skin).
- While these signs of irreversible death would not be expected to be seen in most practice settings, the American Heart Association also includes the following irreversible signs of death:
- decapitation (separation of the head from the body)
- decomposition (decay or putrification of the body)
- rigor mortis (stiffness of the limbs and body that develops 2 - 4 hours after death and may take up to 12 hours to fully develop).
Upon reporting clinical findings to the physician, and in accordance with facility policy, the LVN may accept reasonable physician’s orders regarding the care of the client; i.e.: notification of family, postmortem care, contacting the funeral home or appropriate legal authority, documentation; however, a LVN may not accept an order that would require the LVN to “pronounce death,” or to complete the state-required “medical certification” of a death that occurs without medical attendance.
The BON has no jurisdiction over physician practice, facility policies, or the laws regulating pronouncement of death in Texas. Additional information on Texas regulations regarding pronouncement of death may be found in Chapters 193 and 671 of the Texas Health and Safety Code, as well as through the Department of State Health Services. A LVN is not responsible for the actions of a physician who elects to pronounce death by remote-means. Physicians are licensed by, and must comply with, rules promulgated by the Texas Medical Board as well as other laws applicable to the physician’s practice setting.
References
American Heart Association (2020). American Heart Association CPR & ECC guidelines. Retrieved from https://eccguidelines.heart.org/circulation/cpr-ecc-guidelines/
Texas Health and Safety Code Chapters 193 and 671: http://www.statutes.legis.state.tx.us/
(BVNE Statement adopted 06/1999; Revised BON statement: 01/2006)
(Revised: 01/2007; 01/2008; 01/2009; 01/2011; 01/2012; 01/2013; 01/2014; 01/2015; 01/2016; 01/2018; 01/2019; 01/2021)
(Reviewed: 01/2010; 01/2017)
Return to top
|
15.3 LVNs Engaging in Intravenous Therapy, Venipuncture, or Peripherally Inserted Central Catheter (PICC) Lines
|
|
The basic educational curriculum for Licensed Vocational Nurses (LVNs) does not mandate teaching of principles and techniques for insertion of peripheral intravenous (IV) catheters, or the administration of fluids and medications via the IV route. Knowledge and skills relating to maintaining patency and performing dressing changes of central line IV catheters is also not mandated as part of basic LVN education. As such, it cannot be presumed that all LVN licensees possess basic competency in the management of IV lines/IV therapy.
Applicable Nursing Standards
LVN practice is guided by the Nursing Practice Act (NPA) and Board Rules. 22 TAC §217.11, Standards of Nursing Practice, is the Board rule most often applied to nursing practice issues. Two standards applicable in all practice scenarios include:
- §217.11(1)(B) Implement measures to promote a safe environment for clients and others, and
- §217.11(1)(T) Accept only those nursing assignments that take into consideration client safety and that are commensurate with the nurse’s educational preparation, experience, knowledge, and physical and emotional ability.
Additional standards in 22 TAC §217.11 that may be applicable when an LVN chooses to engage in an IV therapy related task include (but are not limited to):
- (1)(C) Know the rationale for and the effects of medications and treatments and correctly administer the same,
- (1)(D) Accurately and completely report and document: (i) client status...(ii) nursing care rendered...(iii) physician, dentist or podiatrist orders...(iv) administration of medications and treatments...(v) client response(s)...,
- (1)(G) Obtain instruction and supervision as necessary when implementing nursing procedures or practices,
- (1)(H) Make a reasonable effort to obtain orientation/training for competency when encountering new equipment and technology or unfamiliar care situations,
- (1)(R) Be responsible for one’s own continuing competence in nursing practice and individual professional growth,
- (2)(A) Utilize a systematic approach to provide individualized, goal-directed nursing care...[(i)-(v)], and
- (2)(C) ...perform other acts that require education and training as prescribed by board rules and policies, commensurate with the LVN’s experience, continuing education, and demonstrated LVN competencies.
Position Statement 15.27, The Licensed Vocational Nurse Scope of Practice, provides additional clarification of the Standards of Nursing Practice Rule as it applies to LVN scope of practice. Instruction and skill evaluation relating to LVNs performing insertion of peripheral IV catheters and/or administering IV fluids and medications as prescribed by an authorized practitioner may allow a LVN to expand his/her scope of practice to include IV therapy.
It is the opinion of the Board that the LVN shall not engage in IV therapy related to either peripheral or central venous catheters, including venipuncture, administration of IV fluids, and/or administration of IV push medications, until successful completion of a validation course that instructs the LVN in the knowledge and skills applicable to the LVN’s IV therapy practice. The BON does not define or set qualifications for an “IV Validation Course” or for "LVN IV certification." The LVN who chooses to engage in IV therapy must first have been instructed in the principles of IV therapy congruent with prevailing nursing practice standards.
Insertion and Removal of PICC Lines or Midline Catheter
The Board has further determined that vocational nursing programs do not provide the LVN with the educational foundation to assure client safety in insertion and removal of Peripherally Inserted Central Catheters (PICC lines) or midline catheters, inclusive of vein selection, insertion/advancement/retraction of the catheter, determining placement, and monitoring of the client for untoward reactions in relation to catheter insertion and removal. The LVN scope of practice is a directed scope of practice utilizing a focused assessment for patients with predictable healthcare needs. Patients having PICC lines either inserted or removed are at risk for complications, e.g., air embolism, nerve damage, infection1, and could potentially become unpredictable needing a comprehensive assessment, as well as changes to nursing diagnoses and plan of care to ensure vascular access. This position of the Board aligns with boards of nursing across the nation2,3,4,5,6,7,8,9.Position Statement 15.27, The Licensed Vocational Nurse Scope of Practice, and Position Statement 15.10, Continuing Education: Limitations for Expanding Scope of Practice, further maintains that continuing education that falls short of an educational program of study leading to a degree and licensure as a registered nurse would be insufficient to assure vocational nurse competency and patient safety with regard to insertion and removal of PICC lines or midline catheters. Therefore, it is the Board’s position that insertion and removal of PICC lines or midline catheters is beyond the scope of practice for LVNs.1
Administration of IV Fluids and Medications
The ability of an LVN to administer specific IV fluids or drugs, to prepare and/or administer IV “piggy-back” or IV “push” medications, or to monitor and titrate “IV drip” medications of any kind is up to facility policy. The LVN’s practice relative to IV therapy must also comply with any other regulations that may exist under the jurisdiction of other regulatory agencies or entities. The LVN who accepts an assignment to engage in any aspect of IV therapy is responsible for adhering to the NPA and Board rules, particularly 22 TAC §217.11, Standards of Nursing Practice, including excerpted standards listed above and any other standards or rules applicable to the individual LVN’s practice.
All nursing actions related to peripheral and/or central intravenous lines, as well as IV administration of medications, must be completed in accordance with the orders of the prescribing practitioner, as well as written policies, procedures and job descriptions approved by the health care employer.
References
1 Gorski, L., Hadaway, L., Hagle, M. E., McGoldrick, M., Orr, M., & Doellman, D. (2016). Infusion therapy: Standards of practice. Journal of Infusion Nursing 39(1S).
2 Alabama Board of Nursing. (2016). Alabama Board of Nursing approved standardized procedures. Retrieved from https://www.abn.alabama.gov/wp-content/uploads/2016/03/Approved-Standardized-Procedures.pdf
3 Connecticut Board of Examiners for Nursing. (1997). Suggested guidelines for registered nurses in the insertion and removal of specialized intravenous catheters. Retrieved from https://portal.ct.gov/-/media/Departments-and-Agencies/DPH/dph/phho/Nursing_Board/Guidelines/Specialcathpdf.pdf?la=en
4 Iowa Board of Nursing. (2011). Chapter 6: Nursing practice for registered nurses/licensed practical nurses. Retrieved from https://www.legis.iowa.gov/docs/iac/chapter/09-27-2017.655.6.pdf
5 Massachusetts Board of Registration in Nursing. (2015). Peripherally inserted central catheters (PICC). Retrieved from http://www.mass.gov/eohhs/gov/departments/dph/programs/hcq/dhpl/nursing/nursing-practice/advisory-rulings/peripherally-inserted-central-catheters.html
6 Mississippi Board of Nursing. (2000). Insertion, maintenance and removal of peripherally inserted central catheters (PICC). Retrieved from http://www.msbn.ms.gov/Documents/PICC_2000.pdf
7 South Dakota Board of Nursing. (2012). IV therapy education. Retrieved from https://doh.sd.gov/documents/LPNintravenousTherapy.pdf
8 Vermont Board of Nursing. (2012). The role of the license practical nurse in intravenous infusion therapy. Retrieved from https://www.sec.state.vt.us/media/369316/ps-role-of-the-lpn-in-iv-therapy.pdf
9 Wyoming State Board of Nursing. (2017). Advisory Opinion LPN IV certified (IV-C) scope of practice. Retrieved from https://nursing-online.state.wy.us/Resources/AO_LPN%20IV-C%20Scope%20of%20Practice.pdf
(Board Action: 06/1995; Revised: 09/1999; 01/2005; 01/2011; 01/2012; 01/2014; 01/2015; 01/2018; 01/2019; 01/2020)
(Reviewed: 01/2006; 01/2007; 01/2008; 01/2009; 01/2010; 01/2013; 01/2016; 01/2017; 01/2021)
Return to top
|
15.4 Educational Mobility
|
|
The Texas Board of Nursing (Board or BON) supports educational mobility for nurses prepared at the VN, ADN, Diploma and BSN levels and encourages the elimination of needless repetition of experiences or time penalties. Furthermore, the Board encourages existing nursing education programs approved by the Texas Board of Nursing to develop articulation arrangements that specify their policies regarding transfer of academic credits to facilitate educational mobility, especially in underserved areas of the state.
The Board honors and supports military personnel and veterans and their educational mobility. Several Board approved education programs offer articulated credit or other options for military personnel with healthcare training and/or experience.
(Board Action 01/1989)
(Revised: 01/1992; 01/2005; 01/2008; 01/2015; 01/2018)
(Reviewed: 01/2006; 01/2007; 01/2009; 01/2010; 01/2011; 01/2012; 01/2013; 01/2014; 01/2016; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
15.5 Nurses with Responsibility for Initiating Physician Standing Orders
|
|
According to the Texas Nursing Practice Act [Tex. Occ. Code Ann. §301.002(3)], the term "Nurse" means, “a person required to be licensed under this chapter to engage in professional or vocational nursing.” The practice of either professional or vocational nursing frequently involves implementing orders from a physician, podiatrist, or dentist. Timely interventions for various patient populations can be facilitated using physician’s standing orders that authorize the nurse to carry out specific orders for a patient presenting with or developing a condition or symptoms addressed in the standing orders.
The specifics of how authorization occurs for a LVN or RN to implement a set of standing physician’s orders are defined in the Texas Medical Board’s (TMB) Rule 193 (22 Tex. Admin. Code §§193.1-193.20) relating to physician delegation. This rule delineates two methods by which nurses may follow a pre-approved set of orders for treating patients:
- Standing Delegation Orders; and/or
- Standing Medical Orders
These terms are defined in 22 Tex. Admin. Code §193.2 as follows:
(19) Standing delegation order -- Written instructions, orders, rules, regulations, or procedures prepared by a physician and designed for a patient population with specific diseases, disorders, health problems, or sets of symptoms. Such written instructions, orders, rules, regulations or procedures shall delineate under what set of conditions and circumstances action should be instituted. These instructions, orders, rules, regulations or procedures are to provide authority for and a plan for use with patients presenting themselves prior to being examined or evaluated by a physician to assure that such acts are carried out correctly and are distinct from specific orders written for a particular patient, and shall be limited in scope of authority to be delegated as provided in §193.4 of this title (relating to Scope of Standing Delegation Orders). As used in this chapter, standing delegation orders do not refer to treatment programs ordered by a physician following examination or evaluation by a physician, nor to established procedures for providing of care by personnel under direct, personal supervision of a physician who is directly supervising or overseeing the delivery of medical or health care. As used in this chapter, standing delegation orders are separate and distinct from prescriptive authority agreements as defined in this chapter. Such standing delegation orders should be developed and approved by the physician who is responsible for the delivery of medical care covered by the orders.
Such standing delegation orders, at a minimum, should:
- include a written description of the method used in developing and approving them and any revision thereof;
- be in writing, dated, and signed by the physician;
- specify which acts require a particular level of training or licensure and under what circumstances they are to be performed;
- state specific requirements which are to be followed by persons acting under same in performing particular functions;
- specify any experience, training, and/or education requirements for those persons who shall perform such orders;
- establish a method for initial and continuing evaluation of the competence of those authorized to perform same;
- provide for a method of maintaining a written record of those persons authorized to perform same;
- specify the scope of supervision required for performance of same, for example, immediate supervision of a physician;
- set forth any specialized circumstances under which a person performing same is to immediately communicate with the patient's physician concerning the patient's condition;
- state limitations on setting, if any, in which the plan is to be performed;
- specify patient record-keeping requirements which shall, at a minimum, provide for accurate and detailed information regarding each patient visit; personnel involved in treatment and evaluation on each visit; drugs, or medications administered, prescribed or provided; and such other information which is routinely noted on patient charts and files by physicians in their offices; and
- provide for a method of periodic review, which shall be at least annually, of such plan including the effective date of initiation and the date of termination of the plan after which date the physician shall issue a new plan.
(20) Standing medical orders -- Orders, rules, regulations or procedures prepared by a physician or approved by a physician or the medical staff of an institution for patients which have been examined or evaluated by a physician and which are used as a guide in preparation for and carrying out medical or surgical procedures or both. These orders, rules, regulations or procedures are authority and direction for the performance for certain prescribed acts for patients by authorized persons as distinguished from specific orders written for a particular patient or delegation pursuant to a prescriptive authority agreement.
A third term, "Protocols", is defined narrowly by the TMB and applies to RNs with advanced practice licensure (APRN) by the BON, or to Physician Assistants only:
(18) Protocols -- Written authorization delegating authority to initiate medical aspects of patient care, including delegation of the act of prescribing or ordering a drug or device at a facility-based practice. The term protocols is separate and distinct from prescriptive authority agreements as defined under the Act and this chapter. However, prescriptive authority agreements may reference or include the terms of a protocol(s). The protocols must be agreed upon and signed by the physician, the physician assistant and/or advanced practice registered nurse, reviewed and signed at least annually, maintained on site, and must contain a list of the types or categories of dangerous drugs and controlled substances available for prescription, limitations on the number of dosage units and refills permitted, and instructions to be given the patient for follow-up monitoring or contain a list of the types or categories of dangerous drugs and controlled substances that may not be prescribed. Protocols shall be defined to promote the exercise of professional judgment by the advanced practice registered nurse and physician assistant commensurate with their education and experience. The protocols used by a reasonable and prudent physician exercising sound medical judgment need not describe the exact steps that an advanced practice registered nurse or a physician assistant must take with respect to each specific condition, disease, or symptom.
By definition, both vocational and professional nursing excludes “acts of medical diagnosis or the prescription of therapeutic or corrective measures” [Tex. Occ. Code Ann. §301.002(2) and (5)]. Based on the above definitions in the TMB rules, RNs who do not have advanced practice licensure from the BON may not utilize "protocols" to carry out physician orders. Likewise, LVNs are also prohibited from utilizing protocols as defined by the TMB, as neither LVNs nor RNs may engage in acts that require independent medical judgment.
A nurse responsible for initiating physician's standing medical orders or standing delegation orders may select specific tasks or functions for patient management, including the administration of a medication required to implement the selected order provided such selection be within the scope of the standing orders. The selection of such tasks or functions for patient management constitutes a nursing decision that may be carried out by a LVN or RN. In addition, this position statement should not be construed to preclude the use of the term “protocol” for a standard set of orders covering the monitoring and treatment of a given clinical condition (e.g., insulin protocol, heparin protocol, ARDS protocol, etc.) provided said standard orders meet the requirements for standing delegation or standing medical orders as defined by the TMB.
The written standing orders under which nurses function shall be commensurate with each nurse’s educational preparation and experience. The nurse initiating any form of standing orders must act within the scope of the Nursing Practice Act, Board Rules and Regulations, and any other applicable local, state, or federal laws.
(Board Action 07/1988; Revised: 01/1992; 07/2001; 01/2005; 01/2006; 01/2007; 01/2009; 01/2011; 01/2014; 01/2016; 01/2018)
(Reviewed: 01/2008; 01/2010; 01/2012; 01/2013; 01/2015; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
15.6 Board Rules Associated with Alleged Patient "Abandonment"
|
|
The Texas Board of Nursing (BON or Board), in keeping with its mission to protect public health, safety, and welfare, holds nurses accountable for providing a safe environment for patients and others over whom the nurse is responsible [22 TAC §217.11(1)(B)]. Though the Nursing Practice Act (NPA) and Board rules do not define the term “abandonment,” the Board has investigated and disciplined nurses in the past for issues surrounding the concept of abandonment as it relates to the nurse’s duty to a patient. The Board’s position applies to all licensed nurses (LVNs, RNs, and APRNs), including RN’s with advanced practice licensure (Nurse Practitioners, Clinical Nurse Specialists, Nurse Midwives, and Certified Registered Nurse Anesthetists) in Texas.
Nurse’s Duty to a Patient
All nurses, regardless of practice setting or position title/role, are required to adhere to the NPA and Board rules. The “core” rules relating to nursing practice are 22 TAC §217.11, Standards of Nursing Practice, and 22 TAC §217.12, Unprofessional Conduct. The standard upon which all other standards are based is 22 TAC §217.11(1)(B) “...promote a safe environment for clients and others.” This standard supersedes a physician’s order or facility’s policy and has previously been upheld in a landmark case, Lunsford v. Board of Nurse Examiners, 648 S.W. 2d 391 (Tex. App. -- Austin 1983). The concept of the nurse’s duty to promote patient safety also serves as the basis for determining behavior that could be considered unprofessional conduct by a nurse.
Patients under the care of a nurse are vulnerable by virtue of illness, injury, and/or the dependent nature and unequal power base of the nurse-patient relationship. Persons who are especially vulnerable include the elderly, children, the mentally ill, sedated and anesthetized patients, those whose mental or cognitive ability is compromised, and patients who are physically disabled, immobilized, restrained, or secluded. The nurse’s duty to protect the patient is created by the patients' vulnerability and the nurse's power base. The distinction between a nurse leaving employment versus a nurse violating a duty to a patient through leaving an assignment is often confused. The first is an employment issue; the other is potentially a licensure issue.
There is also no routine answer to the question, “When does the nurse’s duty to a patient begin?” The nurse’s duty is not defined by any single event such as clocking in or taking report. From a BON standpoint, the focus for disciplinary sanctions is on the relationship and responsibility of the nurse to the patient, not to the employer or employment setting.
Employment Issues
Though the Board has no jurisdiction over employers or employment-related issues, other laws regulating facility licensure may apply certain responsibilities to the employer for provision of patient safety, such as development of effective patient care systems or provision of adequate numbers of qualified staff. Specific requirements for a given facility may be obtained by contacting the applicable licensing authority for the institution.
The Board believes that the following additional examples of employment issues would not typically involve violations of the NPA or Board Rules:
- resignation without advance notice, assuming the nurse’s current patient care assignment and/or work shift has been completed;
- refusal to work additional shifts, either “doubles” or extra shifts on days off; and/or
- other work-related issues, such as frequent absenteeism or tardiness, or conflicts between staff/employees.
The Board believes nurses should be vigilant and exercise sound professional judgment when accepting assignments that may be requested by employers who need nurses to fill vacant shifts for licensed nursing staff or other staffing-related situations. Clear communication between staff and supervisors is essential to arrive at solutions that best focus on patient care needs without compromising either patient safety or a nurse’s license.
Licensure Issues
As previously noted, the rules most frequently applied to nursing practice concerns are 22 TAC§217.11, Standards of Nursing Practice, and 22 TAC §217.12, Unprofessional Conduct. In relation to questions of "abandonment,” standard 22 TAC §217.11(1)(I) holds the nurse responsible to “notify the appropriate supervisor when leaving a nursing assignment.” This standard should not be misinterpreted to mean a nurse may simply notify the supervisor that he/she is leaving the premises, regardless of whether or not another qualified licensed nurse is available to assume care of the nurse’s patients. Specific procedures to follow in a given circumstance (i.e., nurse becomes ill, family emergency, etc.) should be delineated in facility policies (which the Board does not regulate).
Some actions may be more obvious examples of unprofessional conduct that could result in sanctions on the nurse’s license. Examples of conduct that could lead to Board action on the nurse’s license may include:
- sleeping on the job, which effectively makes the nurse unavailable to observe the patient or respond to the patient’s needs, even though the nurse is physically present;
- simply walking off the job in mid-shift without notifying anyone and without regard for patient safety;
- failing to initiate or complete an agreed assignment when the nurse is the sole care provider, and/or the nurse is a consultant or supervisor in a home or homelike setting; and/or failing to notify a supervisor in a timely manner that the assignment will not be done, and/or falsifying records to the effect that the missed nursing visit was indeed completed; and/or
- leaving the assigned patient care area and remaining gone or unavailable for a period of time such that the care of any/all patients may be compromised due to lack of available licensed staff.
The Board may impose sanctions on a nurse’s license for actions that potentially place patients at risk for harm or when harm has resulted because a nurse violated his or her duty to the patient by leaving a patient care assignment in a manner inconsistent with the Board rules.
Emergency Preparedness
A nurse may have to choose between the duty to provide safe patient care and protecting the nurse’s own life during an emergency, including but not limited to disasters, infectious disease outbreaks or acts of terrorism. The Board believes nurses should be vigilant and exercise sound professional judgment when accepting assignments that may be requested by employers who need nurses to fill vacant shifts for licensed nursing staff or other staffing-related situations. These situations are challenging for all nurses and their employers, therefore the Board recommends policies and procedures be developed, and periodically reviewed, to provide clear guidance and direction to nurses in order for patients to receive safe and effective care. A nurse may have to choose between the duty to provide safe patient care and protecting the nurse's own life during a violent situation that may occur in the workplace. For example, when an active shooter is present in the workplace, the nurse should take steps to protect the patients if there is time and using a method that does not jeopardize the nurse's personal safety or interfere with law enforcement personnel. These steps may include evacuating the area or preventing entry to an area where the active shooter is located. However, during an active shooter situation a nurse may find there is not sufficient time to do anything but to ensure his or her own safety. In this instance, as soon as the situation has resolved the nurse should promptly resume care of patients. Clear communication between staff and supervisors is essential to arrive at solutions that best focus on patient care needs without compromising either patient safety or a nurse’s license.
Board Disciplinary Actions
Complaints of “patient abandonment” when it is obvious from the allegation that it is an employment issue will not be investigated by the Board. In these circumstances, however, both parties (the nurse and the employer) may be advised to strive for alternate solutions to avoid similar situations in the future.
Some general factors that would be considered in investigating a complaint alleging a nurse left an assignment by a nurse would include, but not be limited to:
- the extent of dependency or disability of the patient;
- stability of the patient;
- the length of time the patient was deprived of care;
- any harm to the patient/level of risk of harm to the patient;
- steps taken by the nurse to notify a supervisor of the inability to provide care;
- previous history of leaving a patient-care assignment;
- emergencies that require nurses to respond, including but not limited to disasters, disease outbreaks, and bioterrorism;
- workplace violence, including but not limited to an active shooter situation;
- other unprofessional conduct in relation to the practice of nursing;
- nurse's general competency regarding adherence to minimum nursing standards.
As with all allegations received by the Board, the alleged conduct by a nurse will be thoroughly investigated to determine what, if any, violations of the NPA and rules have occurred. Depending upon the case analysis, Board actions may range from the case being closed with no findings or action all the way to suspension and/or revocation/voluntary surrender of the nurse’s license. If evidence of violations exists, the Board must then determine what level of sanction is appropriate to take on the nurse’s license and what specific stipulation requirements will be applied.
Safe Harbor Nursing Peer Review
If a nurse feels he/she is being asked to accept an assignment that would potentially cause the nurse to violate his/her duty to a patient, the nurse may be able to invoke “safe harbor,” depending on whether or not the nurse’s employer meets requirements that would make it mandatory for the employer to have a nursing peer review plan in place. This is established Chapter 301, Nursing Practice Act; Chapter 303, Nursing Peer Review, and in 22 TAC §217.20, Safe Harbor Peer Review and Whistleblower Protections. Safe harbor has two effects related to the nurse’s license:
- it is a means by which a nurse can request a nursing peer review committee determination of a specific situation in relation to the nurse’s duty to a patient; and
- it affords the nurse immunity from Board action against the nurse’s license if the nurse invokes Safe Harbor in accordance with 22 TAC §217.20. For the nurse to activate this immunity status, the nurse must notify the assigning supervisor at the time the assignment request is made, and the nurse must submit the required information in writing (or verbally if due to immediate patient care needs) to this supervisor, as specified in 22 TAC §217.20(d)(2)(B) & (3) or on the Board’s Safe Harbor Quick Request Form. Do not submit this form to the Board.
Links to related resources:
(Adopted 01/2005; Revised: 01/2006; 01/2007; 01/2009; 01/2011; 01/2014; 01/2015; 01/2017; 01/2018; 01/2019; 01/2021)
(Reviewed: 01/2008; 01/2010; 01/2012; 01/2013; 01/2016; 01/2020)
Return to top
|
15.7 The Role of LVNs & RNs in Management and/or Administration of Medications via Epidural or Intrathecal Catheter Routes
|
|
Role of the LVN
The LVN can provide basic nursing care to patients with epidural or intrathecal catheters. It is the opinion of the Board that the LVN shall not be responsible for the management of a patient's epidural or intrathecal catheter, including administration of any medications via either epidural or intrathecal catheter routes. Management of epidural or intrathecal catheters requires the mastery of complex nursing knowledge and skills that are beyond the competencies of the vocational nursing program or a continuing education course.
Role of the RN
The Board has determined that it may be within the scope of practice of a registered professional nurse to administer analgesic and anesthetic agents via the epidural or intrathecal routes for the purposes of pain control. As with all areas of nursing practice, the RN must apply the Nursing Practice Act (NPA) and Board Rules to the specific practice setting and must utilize good professional judgment in determining whether to engage in a given patient-care related activity.
The Board believes that only licensed anesthesia care providers, as described by the American Society of Anesthesiologists and the American Association of Nurse Anesthetists, as authorized by applicable laws, should perform insertion and verification of epidural or intrathecal catheter placement. Consistent with state law, the attending physician or the qualified provider must order the drugs, dosages, and concentrations of medications to be administered to the patient through the catheter. These interventions are beyond the scope of the registered professional nurse in that independent medical judgment and formal advanced education, skills and training are required to achieve and maintain competence in performing these procedures.
RNs who choose to engage in administration of properly ordered medications via the epidural or intrathecal routes must have documentation that the RN has participated in educational activities to gain and maintain the knowledge and skill necessary to safely administer and monitor patient responses, including the ability to:
- Demonstrate knowledge of the anatomy, physiology, and pharmacology appropriate for administration of medications via the epidural or intrathecal routes;
- Know the medication and medication concentrations approved for use for the specific type of pump;
- Maintain awareness that certain medications are not U.S. Food & Drug Administration (FDA) approved for intrathecal administration (e.g., hydromorphone, bupivacaine, fentanyl, and clonidine);
- Recognize that mixtures of two or more different kinds of medications and compounded medications are not FDA approved for intrathecal administration;
- Anticipate and recognize potential complications of the analgesia relative to the type of infusion device and catheter used;
- Recognize emergency situations and institute appropriate nursing interventions to stabilize the patient and prevent complications;
- Implement appropriate nursing care of patients to include:
- observation and monitoring of sedation levels and other patient parameters;
- administration of medications and monitoring of effectiveness of medication, and catheter monitoring;
- applicable teaching for both patients and their family/significant others related to expected patient outcomes/responses and possible side effects of the medication or treatment; and
- maintenance of the knowledge and skill to remove catheters, when applicable.
Appropriate nursing policies and procedures that address the education and skills of the RN and nursing care of the patient should be developed to guide the RN in the administration of epidural and/or intrathecal medications. RNs and facilities should consider evidence-based practice guidelines put forth by professional specialty organizations(s), such as the American Association of Nurse Anesthetists and the American Society of Anesthesiologists, when developing appropriate guidance for the RN in a particular practice setting. For example, the Association of Women’s Health, Obstetric and Neonatal Nurses’ (AWHONN) has a clinical position statement on "Role of the Registered Nurse in the Care of the Pregnant Woman Receiving Analgesia and Anesthesia by Catheter Techniques." This nationally recognized practice guideline states that it is beyond the scope of practice of the obstetrical nurse to institute or change the rate of continuous infusions via epidural or intrathecal catheters. The American Association of Nurse Anesthetists has a similar position. Nurses should also be aware of FDA safety communications regarding intrathecal administration of pain medication.
The Board encourages the use of the BON’s Scope of Practice Decision-Making Model (DMM) . Finally, standing medical orders approved by the medical and/or anesthesia staff of the facility should include, but not necessarily be limited to, the following:
- The purpose and goal of treatment;
- The dosage range of medication to be administered, including the maximum dosage;
- Intravenous access;
- Treatment of respiratory depression and other side effects, including an order for a narcotic antagonist;
- Options for inadequate pain control; and
- Physician/CRNA availability and backup.
References
American Association of Nurse Anesthetists. (2017). Care of patients receiving analgesia by catheter techniques. Retrieved from https://www.aana.com/docs/default-source/practice-aana-com-web-documents-(all)/care-of-patients-receiving-analgesia-by-catheter-techniques.pdf?sfvrsn=d30049b1_2
Association of Women’s Health, Obstetric, and Neonatal Nurses. (2020). Role of the registered nurse in the care of the pregnant woman receiving analgesia and anesthesia by catheter techniques. Retrieved from https://www.jognn.org/article/S0884-2175(20)30012-5/fulltext
US Food and Drug Administration. (2018). Implanted Pumps: Safety Communication—Use Caution When Selecting Pain Medicine for Intrathecal Administration. Retrieved from:
https://www.fda.gov/medical-devices/safety-communications/use-caution-implanted-pumps-intrathecal-administration-medicines-pain-management-fda-safety
(LVN role: BVNE 1994; Revised BON 01/2005)
(RN role: BON 06/1991; Revised: 01/2003; 01/2004; 01/2005; 01/2011; 01/2014; 01/2016; 01/2018; 01/2019; 01/2020; 01/2021)
(Reviewed: 01/2006; 01/2007; 01/2008; 01/2009; 01/2010; 01/2012; 01/2013; 01/2015; 01/2017)
Return to top
|
15.8 Role of the Nurse in Moderate Sedation
|
|
Note: This position statement is not intended to apply to:
- The practice of the registered nurse who holds licensure as an advanced practice registered nurse in the role and population focus of nurse anesthetist (CRNA) functioning within his/her authorized scope of practice;
- The registered nurse practicing in an acute care setting, such as critical care, where the patient in question is intubated, receiving mechanical ventilatory support, and continuously monitored by the patient care RN; or
- Adjunct or off label use of low dose agents for pain management or other indications.
Role of the LVN
The administration of pharmacologic agents via intravenous or other routes for the purpose of achieving moderate sedation requires mastery of complex nursing knowledge, advanced skills, and the ability to make independent nursing judgments during an unstable and unpredictable period for the patient. It is the opinion of the Board that the one-year vocational nursing program does not provide the Licensed Vocational Nurse (LVN) with the educational foundation to assure patient safety for optimal anesthesia care inclusive of both the administration of pharmacologic agents intended to induce moderate sedation and/or assessment and monitoring of the patient receiving moderate (conscious) sedation.
In alignment with 22 TAC §217.11, Standards of Nursing Practice, Board Position Statement 15.27, The Licensed Vocational Nurse Scope of Practice, and Board Position Statement 15.10, Continuing Education: Limitations for Expanding Scope of Nursing Practice, the Board also maintains that continuing education that falls short of achieving licensure as a registered nurse would be insufficient to assure vocational nurse competency and patient safety with regard to both medication administration and patient monitoring associated with moderate sedation.
Though the Board cannot dictate physician practice, it is the Board’s position that a LVN cannot administer medications or monitor patients receiving moderate sedation as a delegated medical act.
Role of the RN or non-CRNA Advanced Practice Registered Nurse
Though optimal anesthesia care is best provided by qualified certified registered nurse anesthetists (CRNAs) or anesthesiologists, the Board recognizes that the demand in the practice setting necessitates provision of moderate sedation by registered nurses and non-CRNA advanced practice registered nurses in certain practice situations.
All licensed nurses practicing in Texas are required to “know and comply” with the Nursing Practice Act (NPA) and Board Rules. 22 TAC §217.11(1)(B) requires the nurse to “promote a safe environment for clients and others.” This standard establishes the nurse’s duty to the patient/client, which supersedes any physician order or any facility policy. This “duty” to the patient requires the nurse to use informed professional judgment when choosing to assist or engage in a given procedure. [See Position Statement 15.14, Duty of a Nurse in Any Practice Setting].
As the NPA and Board rules are not prescriptive to specific tasks a nurse may or may not perform, a RN or non-CRNA advanced practice registered nurse should consider evidence-based practice guidelines put forth by professional organizations with clinical expertise in the administration of pharmacologic agents used for sedation/anesthesia as well as advanced airway management and cardiovascular support. A number of professional specialty organizations have well-defined standards and recommendations for ongoing nursing education and competency assessment related to administration and monitoring of patients receiving moderate sedation.
These organizations include the American Association of Nurse Anesthetists (AANA)1, the American Nurses Association (ANA)2, the Association of periOperative Registered Nurses (AORN)3, and the Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN).4 Statements published by the American Society of Anesthesiologists (ASA) also support the positions of the above nursing organizations.5 The Board advises the nurse use caution in applying moderate sedation standards of any individual or specialty group who are not also experts in the field of advanced airway management/anesthesia. The Board encourages the use of the BON’s Scope of Practice Decision-Making Model (DMM)
Employing institutions should develop policies and procedures to guide the RN or non-CRNA advanced practice registered nurse in administration of medications and patient monitoring associated with moderate sedation. Policies and procedures should include but not be limited to:
- Performance of a pre-sedation health assessment by the individual ordering the sedation and the RN or non-CRNA advanced practice registered nurse administering the sedation;
- Guidelines for patient monitoring, drug administration, and a plan for managing potential complications or emergency situations developed in accordance with currently accepted standards of practice;
- Accessibility of emergency equipment and supplies;
- Documentation and monitoring of the level of sedation and physiologic measurements (e.g. blood pressure, oxygen saturation, cardiac rate and rhythm); and
- Documentation/evidence of initial education and training and ongoing competence of the RN or non-CRNA advanced practice registered nurse administering and/or monitoring patients receiving moderate sedation
Use of Specific Pharmacologic Agents
It is up to facilities and physicians to determine specific pharmacologic agents to be used to induce moderate sedation. The Board advises the RN or non-CRNA advanced practice registered nurse use caution, however, when deciding whether s/he has the competency to administer the specific pharmacologic agents ordered by the physician. What is within the scope of practice for one RN is not necessarily within the scope of practice for another RN. (See references to 22 TAC §217.11 & Scope of Practice Decision-Making Model (DMM) above). With regard to this issue, the Board recommends the RN also take into consideration:
- Availability of and knowledge regarding the administration of reversal agents for the pharmacologic agents used; and
- If reversal agents do not exist for the pharmacologic agents used or the criteria outlined in (1) above are not met, then the nurse must consider his/her individual knowledge, skills, and abilities to rescue a patient from un-intended deep sedation/anesthesia using advanced life support airway management equipment and techniques.
RNs or non-CRNA Advanced Practice Registered Nurses Administering Propofol, Ketamine, or Other Anesthetic Agents to Non-Intubated Patients
Of concern to the Board is the growing number of inquiries related to RNs and non-CRNA advanced practice registered nurses administering Propofol, Ketamine, or other drugs commonly used for anesthesia purposes to non-intubated patients for the purpose of moderate sedation in a variety of patient care settings. It is critical for any RN who chooses to engage in moderate sedation to appreciate the differences between moderate sedation and deep sedation/anesthesia.
Moderate Sedation versus Deep Sedation Anesthesia
According to the professional literature, "moderate sedation" is defined as a medication-induced, medically controlled state of depressed consciousness. Included in the literature from various professional organizations is the caveat that, while under moderate sedation, the patient at all times retains the ability to independently and continuously maintain a patent airway and cardiovascular function, and is able to respond meaningfully and purposefully to verbal commands, with or without light physical stimulation. Reflex withdrawal to physical stimulation is not considered a purposeful response. Loss of consciousness for patients undergoing moderate sedation should not be the goal and thus pharmacologic agents used should render this result unlikely. If the patient requires painful or repeated stimulation for arousal and/or airway maintenance, this is considered deep sedation.
In a state of deep sedation, the patient’s level of consciousness is depressed, and the patient is likely to require assistance to maintain a patent airway. Deep sedation occurring in a patient who is not appropriately monitored and/or who does not have appropriate airway support may result in a life-threatening emergency for the patient. This is not consistent with the concept of moderate sedation as defined in this position statement or the professional literature and is generally considered to be beyond the scope of practice of the RN.
Although Propofol is classified as a sedative/hypnotic/anesthetic, according to the FDA product information, it is intended for use as an anesthetic agent or for maintaining sedation of an intubated, mechanically ventilated patient. The product information brochure for Propofol further includes a warning that “only persons trained to administer general anesthesia and not involved in the conduct of the surgical/diagnostic procedure should administer Propofol for purposes of general anesthesia or for monitored anesthesia care/sedation.” The clinical effects for patients receiving anesthetic agents such as Propofol may vary widely within a negligible dose range. Though reportedly “short-acting”, it is also noteworthy that there are no reversal agents for Propofol.
As the US Food and Drug Administration (FDA) approves computer-assisted personalized sedation systems, a nurse is encouraged to use the Scope of Practice Decision-Making Model (DMM) to reach a sound decision whether to engage in nursing practice utilizing such a device in accordance with the US FDA approval requirements. US FDA approval requirements for computer-assisted personalized sedation systems include requirements for completion of training in addition to safety requirements, such as the immediate availability of anesthesia providers. A nurse is required to complete training prior to using any computer-assisted personalized sedation system and is encouraged to retain proof of training.
The patient receiving anesthetic agents is at increased risk for loss of consciousness and/or normal protective reflexes, regardless of who is administering this medication. The loss of consciousness and/or protective reflexes may indicate progression into deep sedation and this is not consistent with the concept of moderate sedation outlined in the professional literature.
Though the RN or non-CRNA advanced practice registered nurse may have completed continuing education in advanced cardiac life support (ACLS) and practiced techniques during the training program, this process does not ensure ongoing expertise in airway management and emergency intubation. The American Heart Association (AHA)6 has identified factors that contribute to misplacement of the endotracheal tube during resuscitation including: “inadequate training, lack of experience” and patient characteristics such as physiology and movement. It is also important to note that no continuing education program, including ACLS programs, will ensure that the RN or non-CRNA advanced practice registered nurse has the knowledge, skills and abilities to rescue a patient from deep sedation or general anesthesia. Furthermore, it is the joint position of the AANA and ASA that, “because sedation is a continuum, it is not always possible to predict how an individual patient will respond.” These organizations state only qualified anesthesia providers who are trained in the administration of general anesthesia should administer anesthetic agents, including induction agents.
Therefore, it is the position of the Board that the administration of anesthetic agents (e.g. propofol, methohexital, ketamine, and etomidate) is outside the scope of practice for RNs and non-CRNA advanced practice registered nurses except in the following situations:
- when assisting in the physical presence of a CRNA or anesthesiologist (the CRNA or anesthesiologist may direct the RN to administer anesthetic agents in conjunction with the CRNA or anesthesiologist intubating or otherwise managing the patient’s airway)
- when administering these medications as part of a clinical experience within an advanced educational program of study that prepares the individual for licensure as a nurse anesthetist (i.e. when functioning as a student nurse anesthetist)
- when administering these medications to patients who are intubated and mechanically ventilated in critical care settings
- when assisting an individual with current competence in advanced airway management, including emergency intubation procedures
- when utilizing a US FDA approved computer-assisted personalized sedation system in accordance with the US FDA approval requirements, where appropriate safety requirements are met (such as immediate availability of anesthesia providers) after completing appropriate training.
While the physician or other health care provider performing the procedure may possess the necessary knowledge, skills and abilities to rescue a patient from deep sedation and general anesthesia, it is not prudent to presume this physician will be able to leave the surgical site or abandon the procedure to assist in rescuing the patient. In the case of an appropriately licensed practitioner performing a procedure that can be safely abandoned to rescue or intubate the patient, the RN may administer the anesthetic agent when directed. In this instance, the RN is responsible for accepting the assignment and for knowing the rationale, effects, and correctly administering the medication [22 TAC §217.11 (1)(T) & (1)(C)].
The Board again stresses that the nurse’s duty to assure patient safety [22 TAC §217.11(1)(B)] is an independent obligation under his/her professional licensure that supersedes any physician order or facility policy.7 It is important to note that the nurse’s duty to the patient obligates him/her to decline orders for medications or doses of medications that have the potential to cause the patient to reach a deeper level of sedation or anesthesia. The nurse’s duty is outlined in detail in Board Position Statement 15.14, Duty of a Nurse In Any Practice Setting.
Recommended Reference Document: The American Association of Nurse Anesthetists developed an informational advisory document in 2016 to guide policy development for the safe administration of procedural sedation by a non-anesthesia sedation team in a hospital, ambulatory surgical center, or office setting.1 The anesthetic agents Ketamine and Propofol are both mentioned within the document in the context of procedural sedation.
References
1 The American Association of Nurse Anesthetists. (2016). Non-anesthesia Provider Procedural Sedation and Analgesia: Policy Considerations. Retrieved from https://www.aana.com/docs/default-source/practice-aana-com-web-documents-(all)/non-anesthesia-provider-procedural-sedation-and-analgesia.pdf?sfvrsn=670049b1_
2 American Nurses Association. (2008). Procedural Sedation Consensus Statement. Retrieved from https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/procedural-sedation-consensus-statement
3 The Association of periOperative Registered Nurses. (2017). Patient Care Guidelines: Care of the Patient Receiving Moderate Sedation Analgesia. Retrieved from https://aornguidelines.org/guidelines/content?sectionid=173733727&view=book.
4 Association of Women's Health, Obstetric and Neonatal Nurses. (2020). Role of the registered nurse in the care of the pregnant woman receiving analgesia and anesthesia by catheter techniques. Retrieved from http://www.jognn.org/article/S0884-2175(20)30012-5/fulltext
5 American Association of Nurse Anesthetists and American Society of Anesthesiologists. (2013) AANA–ASA Joint Position Statement Regarding Propofol Administration. Retrieved fromhttps://www.aana.com/docs/default-source/practice-aana-com-web-documents-(all)/aana-asa-propofol-joint-ps.pdf?sfvrsn=f80049b1_2
6 American Heart Association (2020). American Heart Association CPR & ECC guidelines. Retrieved from https://eccguidelines.heart.org/circulation/cpr-ecc-guidelines/
7 Lunsford v. BNE, 648 S.W. 391, (Tex. App–Austin 1983)
Additional Resources
Texas Board of Nursing. (2012). Nurses on guard- best practices in patient safety: Off-label administration of Ketamine for pain management by a nurse. Texas Board of Nursing Bulletin, 43(4), 5-6.
Texas Board of Nursing. (2017). FAQ: Off Label Use of Medication.
(Board Action 01/1992; Revised: 01/2003; 01/2004; 01/2006; 01/2007; 01/2009; 01/2012; 01/2013; 01/2014; 01/2016; 01/2017; 01/2018; 01/2019; 01/2020; 01/2021)
(Reviewed: 01/2008; 01/2010; 01/2011; 01/2015)
Return to top
|
15.9 Performance of Laser Therapy by RNs or LVNs
|
|
The Board of Nursing (BON) recognizes that the use of laser therapy and the technology of laser use have changed rapidly since their introduction for medical purposes. Nurses fulfill many important roles in the use of laser therapies. These roles and functions change based upon the type of treatment and the setting in which the treatment occurs. It may be within the scope of nursing practice to perform the delivery of laser energy on a patient with a valid order providing the nurse has the education, experience, and knowledge to perform the assignment [22 TAC §217.11 (1) (T)]. RNs (including Advanced Practice Registered Nurses practicing within their educated role and population focus) or LVNs, with an appropriate clinical supervisor, who choose to administer laser therapy must know and comply with all applicable laws, rules, and regulations, as well as the Nursing Practice Act (NPA) and Rules of the BON [22 TAC §217.11 (1)(A)].
Additional criteria applicable to the nurse who elects to follow an appropriate order in the use of nonablative laser therapy (such as laser hair removal) include:
- Appropriate education related to use of laser technologies for medical purposes, including laser safety standards of the American National Standards Institute and FDA intended-use labeling parameters;
- The nurse’s education and skill assessment is documented in his/her personnel record;
- The procedure has been ordered by a currently licensed physician, podiatrist, or dentist or by an Advanced Practice Registered Nurse (APRN) or Physician Assistant working in collaboration with one of the aforementioned practitioners; and
- Appropriate medical, nursing, and support service back up is available, since remedies for untoward effects of laser therapy may go beyond the scope of practice of the nurse performing the procedure; and
- Specific regulations related to laser hair removal, including educational requirements for a certificate, may be accessed on the Texas Department of Licensing and Regulation website at https://www.tdlr.texas.gov/las/lasrules.htm
Registered Nurses, including APRNs, cannot delegate any aspects of the use of lasers to unlicensed persons. The nurse is expected to comply with the Nursing Practice Act and Board’s Rules and regulations when carrying out any delegated medical act.
Additional regulations potentially applicable to laser use may include Texas Health and Safety Code, Chapter 401, Subchapter M and the Texas Medical Board Rule 193.17 related to Nonsurgical Medical Cosmetic Procedures.
An additional reference in relation to physician delegation: Position Statement 15.11, Delegated Medical Acts.
(Board Action, 05/1992)
(Revised: 11/1997; 01/2003; 04/2004; 01/2006; 01/2008; 01/2009; 01/2011; 04/2013; 01/2014; 01/2017; 01/2018)
(Reviewed: 01/2005; 01/2007; 01/2010; 01/2012; 01/2015; 01/2016; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
Foundation for Initial Licensure and/or APRN licensure
The Board’s Advisory Committee on Education states in its “Differentiated Essential Competencies (DECs) of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors, October 2010" that: “The curricula of each of the nursing programs differ, and the outcomes of the educational levels dictate a differentiated set of essential competencies of graduates. The competencies of each educational level build upon the previous level.” The National Council of State Boards of Nursing (NCSBN) develops and administers two national nurse licensure examinations; the National Council Licensure Examination for Practical Nurses (NCLEX-PN®) and the National Council Licensure Examination for Registered Nurses (NCLEX-RN®). These two examinations are used by all U.S. state and territorial boards of nursing to test entry-level nursing competence of candidates for licensure as Registered Nurses and as Licensed Practical/Vocational Nurses.
Licensure as an Advanced Practice Registered Nurse (APRN) in Texas requires completion of a master’s or postmaster’s advanced practice program, as well as national certification in the advanced role and population focus. To gain licensure as an APRN in Texas, the nurse must first be licensed as a RN in Texas or have privilege to practice in Texas using a valid, unencumbered RN multistate license from a compact state. The nurse must then submit an application to the Board for licensure in the advanced practice role and population focus.
Limitations of “Continuing Education”
The nursing shortage is creating ever-greater challenges for those who must fill nursing vacancies at all levels of licensure and in various specialties. As efforts to invent new ways to fill this growing void expand, the Board is receiving a growing number of calls to clarify the term “continuing education” in relation to how far a nurse can expand his/her practice with informal continuing education offerings.
The formal education for entry into nursing practice in Texas is differentiated between vocational and professional (registered) nursing. Formalized education for advanced practice also requires completion of a formal program of education in the advanced practice role and population focus at the master’s or postmaster’s level.
The Board believes that for a nurse to successfully make a transition from one level of nursing licensure to the next requires the completion of a formal program of education as defined in the applicable board rule [Board Rules 217.2 and 221.4]. The Board also believes that completion of on-going, informal continuing education offerings, such as workshops or online offerings in a specialty area, serve to expand and maintain the competency of the nurse at the current level of licensure. No amount of informal or on-the-job-training can qualify a LVN to perform the same level of care as the RN. Likewise, the RN cannot engage in aspects of care that require independent medical judgement in a given APRN role and population focus without the formal education, national certification, and proper licensure in that APRN role and population focus.
For example, a LVN with 10 years of home care experience cannot perform the comprehensive assessment and initiate the nursing care plan on a patient newly admitted to the services of a home care agency where the LVN is employed. This is precluded in both BON 22 TAC §217.11 as well as in the home care regulations. Attending a workshop and/or spending time under the supervision of a RN does not qualify the LVN to engage in practice that is designated in statue or rule as being exclusive to the next level of licensure.
Therefore, any nurse, regardless of experience, who engages in nursing practice that would otherwise require a higher level of licensure or a APRN licensure type is practicing outside of his/her scope of practice and may be subject to disciplinary action congruent with the NPA and Rules applicable to LVNs, RNs, and/or RNs with APRN licensure in a given role and population focus.
In summary, a nurse functions under his/her own nursing license and, as such, has a duty to patients that is separate from any employment relationship. In other words, a nurse's duty is to keep a patient safe and uphold the standards of nursing practice. A nurse never works under the license of another provider. The nurse must individually assess his/her own education, training, experience, knowledge, abilities, and employment setting policies to determine if the act or task is within his/her scope of practice, and take accountability for acceptance of the assignment and the resultant patient outcomes.
(Adopted 01/2005; Revised: 01/2009; 01/2011; 01/2013; 01/2014; 01/2017; 01/2018; 01/2020)
(Reviewed: 01/2006; 01/2007; 01/2008; 01/2010; 01/2012; 01/2015; 01/2016; 01/2019; 01/2021)
Return to top
|
|
|
|
In carrying out orders from physicians, podiatrists, or dentists for the administration of medications or treatments, nurses are usually engaged in the practice of vocational or professional nursing in accordance with the applicable licensure of the individual nurse. In carrying out some physician orders, however, LVNs or RNs may perform acts not usually considered to be within the scope of vocational or professional nursing practice, respectively. Such tasks are delegated and supervised by physicians, podiatrists, or dentists. RNs who lack licensure as advanced practice registered nurses in a specified role and population focus, and LVNs may not engage in "acts of medical diagnosis or prescription of therapeutic or corrective measures" [NPA, Section 301.002(2) and (5)] as these acts require independent medical judgment, which is beyond the scope of practice of the vocational or registered nurse.
In carrying out the delegated medical function, the nurse is expected to comply with the Standards of Nursing Practice just as if performing a nursing procedure. The Board's position is that a LVN or RN may carry out a delegated medical act if the following criteria are met:
- The nurse has received appropriate education and supervised practice, is competent to perform the procedure safely, and can respond appropriately to complications and/or untoward effects of the delegated medical act [refer to Standards in 22 TAC §217.11 (1)(C), (1)(G), (1)(M), (1)(N), (1)(R), and (1)(T)];
- The nurse’s education and skills assessment are documented in his/her personnel record;
- The nursing and medical staffs have collaborated in the development of written policies/procedures/practice guidelines for the delegated acts, these are available to nursing staff practicing in the facility, and the guidelines are reviewed annually, if applicable;
- The procedure has been ordered by an appropriate licensed practitioner; and
- Appropriate medical and nursing support is available.
The Board recognizes that nursing practice is dynamic and that acts which today may be considered delegated medical acts may in the future be considered within the scope of either vocational or professional nursing practice. The Board, therefore, advises nurses that they must comply with the Board's Standards of Nursing Practice and any other applicable regulations when carrying out nursing and/or delegated medical acts.
(Board Action 09/1993)
(Revised: 03/1994; 01/2001; 01/2003; 01/2004; 01/2005; 01/2011; 01/2014; 01/2017; 01/2018)
(Reviewed: 01/2006; 01/2007; 01/2008; 01/2009; 01/2010; 01/2012; 01/2013; 01/2015; 01/2016; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
The Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnoses are multi-disciplinary psychiatric diagnoses used for the purpose of applying objective criteria, establishing a practice framework and communicating findings with other health care professionals. The current version is the DSM-5 (Fifth Edition).
In accordance with the Nursing Practice Act (NPA), Section 301.002(2) and (5), acts of medical diagnosis or prescription of therapeutic or corrective measures are beyond the scope of practice for licensed vocational nurses as well as registered nurses who are not licensed in an appropriate advanced practice registered nurse (APRN) role and population focus.
The use of DSM-5 diagnoses by a registered nurse licensed by the Board as an APRN in the role and population focus of either a Clinical Nurse Specialist (CNS) in Psychiatric/Mental Health Nursing or as a Psychiatric/Mental Health Nurse Practitioner is authorized provided he/she is acting within the scope of his/her advanced practice role and population focus and that the diagnoses utilized are appropriate for the individual APRN’s advanced education, experience, and scope of practice. APRNs must utilize protocols or other written authorization when providing medical aspects of patient care in compliance with 22 TAC §221, Advanced Practice Nurses. When psychiatric patient conditions are identified that are outside the psychiatric mental health CNS'/NP's scope of practice or expertise, a referral to the appropriate psychiatric mental health or medical provider is indicated.
(Board Action: 09/1996)
(Revised: 01/2005; 01/2006; 01/2008; 01/2009; 01/2010; 01/2011; 01/2014; 01/2015; 01/2016; 01/2017; 01/2018)
(Reviewed: 01/2007; 01/2012; 01/2013; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
The Board of Nursing (BON of Board) recognizes the complexity of nursing in the school health setting and the need to protect the youth of Texas. Although students come to school with complex and diverse health care needs, they should be provided an education in the least restrictive environment. The BON recognizes that the school children of Texas have the right to receive safe, appropriate, and specialized health services that may be required to assure the child's inclusion in the school environment.
Registered Nurses in the School Setting
The Texas Education Agency defines a school nurse in 19 Texas Administrative Code (TAC) § 153.1022 (a) (1) (D) as “… an educator employed to provide full-time nursing and health care services and who meets all the requirements to practice as a registered nurse (RN) pursuant to the Nursing Practice Act and rules and regulations relating to professional nurse education, licensure, and practice and has been issued a license to practice professional nursing in Texas.” The BON believes that school nursing is a professional registered nursing (RN) specialty. School nursing requires comprehensive assessment skills to promote student health, prevent illness and intervene in accordance with the nursing care plan. The RN has the educational preparation and critical thinking skills as well as clinical expertise that are essential to nursing in the school setting. These activities involve the comprehensive assessment of the nursing/health care needs of the student, the development of a nursing plan of care, implementation of the plan, and evaluation of the outcomes. The provision of these services by the RN contributes directly to the students' education and to the successful outcome of the educational process. These essential components of professional nursing practice are the responsibility of the RN in compliance with 22 TAC §217.11(3)(A).
Vocational Nurses in the School Setting
The licensed vocational nurse (LVN) has a directed scope of practice under supervision of a registered nurse, advanced practice registered nurse, physician, physician assistant, podiatrist, or dentist. 1 The provision of nursing care when provided by an LVN in a school setting should be under the supervision of an RN. The RN, in compliance with the BON's Standards of Nursing Practice [22 TAC §217.11], assigns those aspects of care and activities to the LVN that are within the LVN's educational preparation and demonstrated competency to provide. The RN monitors, coordinates, and evaluates the provision of health services necessary to meet individual student health needs essential in achieving educational objectives.
When LVNs are utilized in the school setting and are supervised by the RN, the RN needs to consider how closely they can supervise the LVN and how the RN will direct, guide, and influence the outcome of the LVN’s performance4 and respond to any situations where the LVN needs onsite supervision.2
RN Delegation to Unlicensed Personnel
Due to the growing number of students entering the school system with special health care needs, the BON recognizes that not all health-related services can be provided by a RN or LVN. Therefore, the RN may delegate tasks in the school setting in compliance with the BON's Delegation Rules located in Chapters 224 and 225. School is considered an independent living environment as defined in Chapter 2253; however, acute or emergency situations in the school setting may be delegated in accordance with the rules in both Chapter 224 and Chapter 225. The RN may decide to delegate to an unlicensed person the emergency administration of medications or treatments. Examples include, but are not limited to, Epi-pens, Glucagon, Diastat, oxygen, metered dose inhalers or nebulizer treatments for the relief of acute respiratory symptoms, and the use of a hand held magnet to activate a vagus nerve stimulator to prevent or control seizure activity. All delegation of this nature must be in compliance with 22 TAC §224.6(4) in order to stabilize the child and prevent complications from delaying treatment. The decision to delegate a specific task is always at the discretion of the RN in accordance with 22 TAC §224.8(b)(1)(C) or 22 TAC §225.9(d). Additional delegation resources for RNs can be found in the School Nurse Delegation section of the Delegation Resource Packet of the BON website.
Other Laws Impacting School Health Care
In a school setting, the administration of medication may be assigned to an unlicensed person by the public school official in accordance with the Texas Education Code. The RN's obligation under 22 TAC §225.14 is to verify the training of the unlicensed person, verify the competency of the unlicensed person to perform the task safely, and provide adequate supervision. If the RN is unable to assure these criteria have been met, the RN must notify the public school official.
Summary
Given the complexity, the current number, and the future projections of increasing numbers of children entering the school system with complex nursing and health-related needs, the BON believes that the RN must establish an individualized nursing care plan for each child as applicable. The RN may be assisted by LVNs and unlicensed assistive personnel in the delivery of services to ensure the delivery of safe, effective health care to the school children of Texas.
References
1 Nursing Practice Act, TOC §301.353 and 22 TAC§ 217.11(2)
2 22 TAC§217.11(2)
3 22 TAC §225.4(9)
(Adopted 11/1996; Revised: 11/1997; 01/2003; 01/2005; 01/2008; 01/2009; 01/2011; 01/2013; 07/2013; 01/2016; 01/2018; 1/2019)
(Reviewed: 01/2006; 01/2007; 01/2010; 01/2012; 01/2014; 01/2015; 01/2017; 01/2020; 01/2021)
Return to top
|
|
|
|
In a time when cost consciousness and a drive for increasing productivity have brought about the reorganization and restructuring of health care delivery systems, the effects of these new delivery systems on the safety of clients/patients have placed a greater burden on the licensed vocational nurse (LVN) and the registered professional nurse (RN) to consider the meaning of licensure and assurance of quality care that it provides.
In the interest of fulfilling its mission to protect the health, safety, and welfare of the people of Texas through the regulation of nurses, the Board of Nursing (Board or BON), through the Nursing Practice Act and Board Rules, emphasizes the nurse’s responsibility and duty to the client/patient to provide safe, effective nursing care.
Specifically, the following portions of the Board Rules and supporting documents underscore the duty and responsibilities of the LVN and/or the RN to the client/patient:
- The Standards of Nursing Practice differentiate the roles of the LVN and the RN in accepting nursing care assignments, assuring a safe environment for patients, and obtaining instruction and supervision as needed (22 TAC §217.11); and
- In Lunsford v. Board of Nurse Examiners, 648 S.W. 2d 391 (Tex. App.--Austin, 1983), the court in affirming the disciplinary action of the Board, held that a nurse has a duty to the patient which cannot be superseded by hospital policy or physician's order.
- This landmark case involved a gentleman who arrived to a rural hospital via private vehicle. The gentleman was experiencing severe chest pain, nausea, and sweating—all hallmark symptoms of myocardial infarction (heart attack). Nurse Lunsford was summoned to the ER waiting room by this gentleman’s friend. Upon seeing the acute distress the man was experiencing and hearing his symptoms, she instructed his friend to drive the man to the nearest facility equipped to handle heart attack victims. This facility was 24 miles away. The man succumbed to the heart attack 5 miles away from the small hospital.
- When the Board sought to sanction the nurse’s license, the nurse maintained that the ER physician (who never saw the man) told her the man needed to be transported to the larger facility. The facility policy was also to transfer patients experiencing heart attacks (via ambulance) to the larger facility that was equipped to provide the broad range of therapies that might be needed.
- The court sided with the BON and agreed that the nurse had the knowledge, skills and abilities to recognize the life-threatening nature of the man’s symptoms. Because of this knowledge, the court maintained that it was the nurse’s duty to act in the best interest of the client by assessing the man, taking measures to stabilize him and to prevent complications, and communicating his condition to other staff (such as the physician) to enlist appropriate medical care.
- The Board’s Disciplinary Sanction Policies discuss expectations of all nurses regarding behaviors that are consistent with the Board’s rules 22 TAC §§213.27-213.29. These policies explain the client’s vulnerability and the nurse’s “power” differential over the client by virtue of the client’s status (with regard to age, illness, mental infirmity, etc.) and by the nature of the nurse client relationship (where the client typically defers decisions to the nurse, and relies on the nurse to protect the client from harm).
- The delegation rules guide the RN in delegation of tasks to unlicensed assistive personnel who are utilized to enhance the contribution of the RN to the client's/patient's wellbeing. When performing nursing tasks, the unlicensed person cannot function independently and functions only under the RN's delegation and supervision. Through delegation, the RN retains responsibility and accountability for care rendered (22 TAC Chapters 224 and 225). The Board may take disciplinary action against the license of a RN or RN administrator for inappropriate delegation.
- RNs with advanced practice licensure from the Board must comply with the same rules applicable to other RNs. In addition, rules specific to advanced practice nursing Chapters 221 & 222, as well as laws applicable to the APRN’s practice setting that are outside of the BON’s jurisdiction must also be followed.
- Each nurse must be able to support how his/her clinical judgments and nursing actions are aligned with the NPA and Board Rules. The Board recommends nurses use the Scope of Practice Decision-Making Model (DMM) when trying to determine if a given task is within the individual nurse’s abilities. Congruence with standards adopted by national nursing specialty organizations may further serve to enhance and support the nurse’s decision to perform a particular task.
The nurse, by virtue of a rigorous process of education and examination leading to either LVN or RN licensure, is accountable to the Board to assure that nursing care meets standards of safety and effectiveness.
Therefore, it is the position of the Board that each licensed nurse upholds his/her duty to maintain client safety by practicing within the parameters of the NPA and Board Rules as they apply to each licensee.
Position Statement 15.14 - Duty of a Nurse - DADS QMP poster
(Adopted 01/2005; Revised: 01/2007; 01/2009; 01/2014; 01/2018)
(Reviewed: 01/2006; 01/2008; 01/2010; 01/2011; 01/2012; 01/2013; 01/2015; 01/2016; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
An individual who holds licensure as a licensed vocational nurse (LVN) or as a registered professional nurse (RN) or as an advanced practice registered nurse (APRN) in Texas is responsible and accountable to adhere to the Nursing Practice Act and Board Rules which have the force of law with regard to licensed nursing practice in the state of Texas. Standards of Nursing Practice [22 TAC§217.11(1)(T)] require that each nurse practice within the level of his/her educational preparation, experience, knowledge, and physical and emotional ability. The Standards of Nursing Practice establish the nurse’s duty to the client. This “duty” requires the nurse to intervene appropriately to protect and promote the health and wellbeing of the client or others for whom the nurse is responsible [22 TAC§217.11(1)(B)].
RNs or LVNs Functioning in Unlicensed Positions/Nurse Functioning in another Role
The Nursing Practice Act (NPA) and Board Rules do not preclude a LVN or RN, including a RN/APRN, from seeking employment in unlicensed or technical positions, or in roles the nurse has the knowledge, education, experience, and a valid certificate or license to perform. However, a nurse, who is also licensed by another state agency, is required to comply with the NPA and Board Rules for any acts that are also within the scope of nursing practice [Tex. Occ. Code Ann. § 301.004 (a) (5)]. The Board holds a licensed registered professional nurse, who is working in an unlicensed or technical position, or other role, responsible and accountable to the level of education and competency of a RN. Likewise, a LVN working as an unlicensed or technical person, or in another role, is responsible and accountable to the educational preparation and knowledge of a LVN. This expectation does not apply to individuals formerly licensed as LVNs or RNs or APRNs whose nursing license has been retired, placed on inactive status, surrendered, or revoked.
Use of the Title “LVN” or "RN" when Providing Related Services
The use of the titles “Licensed Vocational Nurse,” or “LVN,” or "Registered Nurse," “RN,” or any designation tending to imply that one is a licensed nurse is limited to those individuals appropriately licensed by the Board. The use of titles implying that an individual holds licensure as a nurse in the State of Texas is restricted by law (Tex. Occ. Code Ann. § 301.351, and Board Rule, 22 Tex. Admin. Code § 217.10). A RN is not automatically a LVN and may not use the title LVN unless the RN also holds an active LVN license. The dually licensed RN/LVN will be held to the standards of the RN license even when working as an LVN. The dually licensed RN/APRN will be held to the nursing standards applicable to the APRN role and population focus when working as an RN in that role and population focus. Use of any protected nursing title by an individual who is not licensed to practice either licensed vocational nursing or professional nursing in accordance with the licensing requirements in Texas, or who does not hold a valid compact license to practice nursing poses a potential threat to public safety related to this act of deception and misrepresentation to the public who may be seeking the services of a licensed nurse.
In the opinion of the Board, the expressed or implied use of the title “LVN,” or "RN," or any other title that implies nursing licensure requires compliance with the NPA and Board Rules. As stated in Rule 217.11(1)(A), the nurse is accountable to adhere to any state, local, or federal laws impacting the nurse’s area of practice.
(Board Action 09/1998)
(Revised: 01/2001; 01/2003; 01/2004; 01/2005; 01/2008; 01/2013; 01/2014; 01/2018)
(Reviewed: 01/2006; 01/2007; 01/2009; 01/2010; 01/2011; 01/2012; 01/2015; 01/2016; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
Approval of nursing education programs is one of the primary functions of the Texas Board of Nursing (Board or BON) in fulfilling its mission to protect and promote the welfare of the people of Texas. The Texas BON has the responsibility and legal authority to decide whether a proposed new nursing education program meets the Board’s established minimum standards for education programs. These standards require adequate human, fiscal, and physical resources, including qualified nursing faculty and clinical learning facilities, to initiate and sustain a program that prepares graduates to practice competently and safely as nurses.
The Texas BON recognizes that when health care facilities experience difficulties in recruiting and retaining sufficient nurses, education institutions and facilities within the affected geographical region frequently respond to this workforce need by proposing new nursing education programs.
Guidelines for Establishing a New Vocational or Professional Nursing Education Program
Entities desiring to start a nursing education program that are not approved as a school/college, must establish a school/college identity and be approved by the Texas Workforce Commission (TWC) as a career school or college (proprietary school) prior to seeking approval for the proposed nursing education program.
All new pre-licensure vocational and professional nursing education programs in Texas must be approved/licensed by either the TWC or the Texas Higher Education Coordinating Board (THECB), as applicable, unless deemed exempt from approval/licensing by the TWC or the THECB; and must also be approved by the Texas BON before enrolling students in the program. A new nursing education program that is deemed exempt from approval/licensing by the TWC or THECB, must still be approved by the Texas BON before enrolling students in the program.
Process for Proposal Approval/Denial
A proposal to establish a new vocational nursing education program or a new professional nursing education program must follow Texas BON Rules & Regulations in Chapter 214 for Vocational Nursing Education or Chapter 215 for Professional Nursing Education. The entity seeking to establish the new program must have the appropriate accreditation/approval and the proposal must be prepared by an individual qualified and designated as the proposed program director. The proposal should include, but not be limited to, extensive rationale which supports establishing the new program with demographic and community data, employment needs for nurses in the area, evidence of support from stakeholders, established agreements with clinical affiliating agencies, adequate qualified nursing administrator and faculty to begin the program, and an acceptable curriculum as identified in the guidelines. The Texas BON Education Guidelines for developing a proposal to establish a new program and a New Proposal Resource Packet are available on the Texas BON web site under the Nursing Education link. An initial approval fee shall be submitted with the proposal [Rule 223.1(a)(9)].
The process for proposal approval/denial begins when the Board staff receives a letter of intent or an initial proposal from the school/college. A program is allowed up to one year from the date of receipt of the proposal in the Board office to finalize all aspects of the proposal for presentation to the Board. The actual length of time until Board approval depends upon the completeness of the proposal and compliance with Board standards. A timeline is included in the Resource Packet. The proposed director should attend at least one Informal Information Session for Proposal Development. The Informal Information Session is provided by board staff several times each year. Representatives from the institution should also attend at least one regularly scheduled Board meeting in order to gain familiarity with Board proceedings.
After the proposal is determined to be ready to be presented to the Board, a preliminary survey visit will be conducted by board staff. The equipment and educational spaces in the physical facility should be ready for the program to begin at this time.
A public hearing will be held at the Board meeting prior to the Board’s discussion of the proposal and the Board’s decision. The Board may approve the proposal and grant initial approval to the new program, may defer action on the proposal, or may deny further consideration of the proposal.
(Board Action 07/2000)
(Revised: 01/2004; 01/2005; 01/2006; 01/2008; 10/2008; 01/2011; 01/2013; 01/2017; 01/2018)
(Reviewed: 01/2007; 01/2009; 01/2010; 01/2012; 01/2014; 01/2015; 01/2016; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
Medication errors occur when a drug has been inappropriately prescribed, dispensed, or administered. Medication errors are a multifaceted problem that may occur in any health care setting. Consistent with their common mission to promote and protect the welfare of the people of Texas, the Board of Nursing and the Board of Pharmacy issued this joint statement for the purpose of increasing awareness of some of the factors which contribute to medication errors.
The Boards note that there are numerous publications available which examine the many facets of this problem, and agree that all elements must be examined in order to identify and successfully correct the problem. This position paper has been jointly developed because the Boards acknowledge the interdisciplinary nature of medication errors and the variety of settings in which these errors may occur. These settings may include hospitals, community pharmacies, doctors' offices/clinics, long-term care facilities, clients' homes, and other locations.
Traditionally, medication errors have been attributed to the individual practitioner. However, reports such as the Institute of Medicine's 1999 report entitled "To Err Is Human: Building a Safer Health System," suggest the majority of medical errors do not result from individual recklessness, but from basic flaws in the way the health system is organized. It is the joint position of the Boards that a comprehensive and varied approach is necessary to reduce the occurrence of errors. The Boards agree that a comprehensive approach includes three major elements: (1) the individual professional's knowledge of practice; (2) resources available to the professional; and (3) systems designs, problems and failures. Each of these three elements of this comprehensive approach are discussed below.
Professional competence has long been targeted as a source of health care professional errors. To reduce the probability of errors, all professionals must accept only those assignments for which they have the appropriate education and which they can safely perform. Professionals must continually expand their knowledge and remain current in their specialty, as well as be alerted to new medications, technologies and procedures in their work settings. Professionals must be able to identify when they need assistance, and then seek appropriate instruction and clarification. Professionals should evaluate strengths and weaknesses in their practice and strive to improve performance. This ultimate accountability on the part of individual practitioners is a critical element in reducing the incidence of medication errors.
The second element (resources available to all professionals) centers on the concept of teamwork and the work environment. The team should be defined as all health care personnel within any setting. Health care professionals must not be reluctant to seek out and utilize each other as resources. This is especially important for the new professional and/or the professional in transition. Taking the time to learn about the resources available in any practice setting is the individual professional's responsibility, and can help decrease the occurrence of medication errors. Adequate staffing and availability of experienced professionals are key factors in the delivery of safe effective medication therapy. In addition, health care organizations have the responsibility to develop complete and thorough orientation for all employees, maintain adequate and updated policies and procedures as guidelines for practice, and offer relevant opportunities for continuing staff development.
Analysis of the third element (systems designs, problems and failures) may demand creative and/or innovative thinking specific to each setting as well as a commitment to guarantee client safety. Systems which may have been in place for a long period of time may need to be re-examined for effectiveness. New information and technological advances must always be taken into account, and input should be solicited from all professionals. In addition, the system should contain a comprehensive quality program for the purpose of detecting and preventing problems and failures. The quality program must encourage all health care professionals to be alert for problems encountered in their daily tasks and to advocate for changes when necessary. In addition, the quality program should include a method of reporting all errors and problems within the system, a system for tracking and analysis of the errors, and an interdisciplinary review of the incident(s). Eliminating systems problems is vital in promoting optimal performance. The table on the following page, while not an exhaustive list, specifies areas that can be reviewed when medication errors occur. These areas encompass all three of the aforementioned contributing elements to the problem of medication errors and can be applied to individuals or systems. Communication is a common thread basic to all of these factors. Effective verbal or written communication is fundamental to successfully resolving breakdowns, either individual or system wide, that frequently contribute to medication errors.
The Boards agree that health care regulatory entities must remain focused on public safety. It is imperative that laws and rules are relevant to today's practice environment and that appropriate mechanisms are in place to address medication errors. The complex nature of the problem requires that there be a comprehensive approach to reducing these errors. It is vital to the public welfare that medication errors be identified, addressed, and reduced.
To view and print the Table: Factors Contributing to Medication Errors in PDF format, click here.
 References
References
Institute of Medicine. (1999). To err is human: Building a safer health system. Washington, D.C.: National Academy Press.
Joint Commission on Accreditation of Healthcare Organizations. (1999, November 19). High-alert medications and patient safety. Sentinel Event Alert, 11, [On-line]. Retrieved from https://www.jointcommission.org/assets/1/18/SEA_11.pdf
Leape, L. L. (1994). Error in medicine. Journal of the American Medical Association, 272(23), 1851-1857.
Nursing Practice Act, TOC Chapters 301 and 303. Texas Pharmacy Act.
TOC, Chapters 551 - 566.
(Board Action 10/2000; 01/2017; 01/2018)
(Reviewed: 01/2005; 01/2006; 01/2007; 01/2008; 01/2009; 01/2010; 01/2011; 01/2012; 01/2013; 01/2014; 01/2015; 01/2016; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
Advanced practice registered nurses (APRNs) are registered nurses who hold licensure from the Texas Board of Nursing to practice as advanced practice registered nurses based on completion of an advanced educational program acceptable to the Board. The term includes a nurse practitioner, nurse-midwife, nurse anesthetist, and a clinical nurse specialist. The advanced practice registered nurse is prepared to practice in an expanded role to provide health care to individuals, families, and/or groups in a variety of settings, including, but not limited to, homes, hospitals, institutions, offices, industry, schools, community agencies, public and private clinics, and private practice. The advanced practice registered nurse acts independently, under the delegated authority of a physician and/or in collaboration with other health care professionals in the delivery of health care services. Advanced practice registered nurses utilize mechanisms, including Protocols, prescriptive authority agreements, or other written authorization, that provide them with the authority to provide medical aspects of care, including the ordering of dangerous drugs, controlled substances, or devices that bear or are required to bear the legend: "Caution: federal law prohibits dispensing without a prescription" or "RX only" or any other legend that complies with federal law. The Protocols, prescriptive authority agreements, or other written authorization may vary in complexity based on the educational preparation and advanced practice experience of the individual advanced practice registered nurse. Protocols, prescriptive authority agreements, or other written authorization are not required to describe the exact steps that an advanced practice registered nurse must take with respect to each specific condition, disease, or symptom. Protocols, prescriptive authority agreements, or other written authorizations are not required for nursing aspects of care.
The Board recognizes that in many settings, nurses and advanced practice registered nurses work together in a collegial relationship. A nurse may carry out an advanced practice registered nurse’s order in the management of a patient, including, but not limited to, the administration of treatments, orders for laboratory or diagnostic testing, or medication orders. A physician is not required to be physically present at the location where the advanced practice registered nurse is providing care. The order is not required to be countersigned by the physician. The advanced practice registered nurse must function within the accepted scope of practice of the role and population focus in which he/she has been licensed by the Board.
As with any order, the nurse must seek clarification if he/she believes the order is inappropriate, inaccurate, non-efficacious or contraindicated by consulting with the advanced practice registered nurse or the physician as appropriate. The nurse carrying out an order from an advanced practice registered nurse is responsible and accountable for his/her actions just as he/she would be with any physician order.
(Board Action: 01/2001)
(Revised: 01/2005; 01/2009; 01/2012; 01/2014; 01/2018)
(Reviewed: 01/2006; 01/2007; 01/2008; 01/2010; 01/2011; 01/2013; 01/2015; 01/2016; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
In response to Senate Bill 659 enacted in 1995 during the 74th Legislative Session, the Texas State Board of Pharmacy and the Texas Medical Board (TMB) entered into a joint rule-making effort to delineate the processes by which a pharmacist could engage in drug therapy management (DTM) as delegated by a physician. The result of this joint effort was the adoption of rules by both the Pharmacy Board [22 TAC §295.13, 1997], and the Texas Medical Board [22 TAC §193.7, 1999]. The TMB amended its rules subsequent to the adoption of §157.101 Delegation to Pharmacist, in the Medical Practice Act during the 76th Legislative Session (1999).
According to definitions listed in the Pharmacy Act [Tex. Occ. Code Ann. §551.003], the “Practice of Pharmacy" includes "(F) performing for a patient a specific act of drug therapy management delegated to a pharmacist by a written protocol from a physician licensed in this state in compliance with Subtitle B." The Pharmacy rules further define DTM as ""the performance of specific acts by pharmacists as authorized by a physician through written protocol. Drug therapy management does not include the selection of drug products not prescribed by the physician, unless the drug product is named in the physician initiated protocol or the physician initiated record of deviation from a standing protocol. Drug therapy management may include the following:
(A) collecting and reviewing patient drug use histories;
(B) ordering or performing routine drug therapy related patient assessment procedures including temperature, pulse, and respiration;
(C) ordering drug therapy related laboratory tests;
(D) implementing or modifying drug therapy following diagnosis, initial patient assessment, and ordering of drug therapy by a physician as detailed in the protocol; or
(E) any other drug therapy related act delegated by a physician” [22 TAC §295.13(b)(4)].
Rule 295.13(b)(6) further adds the clarification that a written protocol is
a physician’s order, standing medical order, standing delegation order, or other order or protocol as defined by rule of the Texas Medical Board under the Medical Practice Act.
(A) A written protocol must contain at a minimum the following:
(i) a statement identifying the individual physician authorized to prescribe drugs and responsible for the delegation of drug therapy management;
(ii) a statement identifying the individual pharmacist authorized to dispense drugs and to engage in drug therapy management as delegated by the physician;
(iii) a statement identifying the types of drug therapy management decisions that the pharmacist is authorized to make which shall include:
(I) a statement of the ailments or diseases involved, drugs, and types of drug therapy management authorized; and
(II) a specific statement of the procedures, decision criteria, or plan the pharmacist shall follow when exercising drug therapy management authority;
(iv) a statement of the activities the pharmacist shall follow in the course of exercising drug therapy management authority, including the method for documenting decisions made and a plan for communication or feedback to the authorizing physician concerning specific decisions made. Documentation shall be recorded within a reasonable time of each intervention and may be performed on the patient medication record, patient medical chart, or in a separate log book; and
(v) a statement that describes appropriate mechanisms and time schedule for the pharmacist to report to the physician monitoring the pharmacist's exercise of delegated drug therapy management and the results of the drug therapy management.
(B) A standard protocol may be used or the attending physician may develop a drug therapy management protocol for the individual patient. If a standard protocol is used, the physician shall record what deviations, if any, from the standard protocol are ordered for that patient.
The TMB Rule [22 TAC §193.15] reflects similar language to the Pharmacy Board rules.
Nurses frequently communicate and collaborate with both the client’s physician and the pharmacist in providing optimal care to clients. It is, therefore, the Board’s position that a nurse may carry out orders written by a pharmacist for DTM provided the order originates from a written protocol authorized by a physician. Any nurse carrying out DTM orders from a pharmacist may wish to review the TMB Rule193, Physician Delegation, in its entirety. The components of the rule related to physician delegation for a pharmacist to engage in DTM are set forth in §193.15(e) as follows:
- A written protocol must contain at a minimum the following listed in subparagraphs (A)-(E) of this paragraph:
- a statement identifying the individual physician authorized to prescribe drugs and responsible for the delegation of drug therapy management;
- a statement identifying the individual pharmacist authorized to dispense drugs and to engage in drug therapy management as delegated by the physician;
- a statement identifying the types of drug therapy management decisions that the pharmacist is authorized to make which shall include:
- a statement of the ailments or diseases, drugs, and type of drug therapy management authorized; and
- a specific statement of the procedures, decision criteria, or plan the pharmacist shall follow when exercising drug therapy management authority;
- a statement of the activities the pharmacist shall follow in the course of exercising drug therapy management authority, including the method for documenting decisions made and a plan for communication or feedback to the authorizing physician concerning specific decisions made. Documentation shall be recorded within a reasonable time of each intervention and may be performed on the patient medication record, patient medical chart, or in a separate log book; and
- a statement that describes appropriate mechanisms and time schedule for the pharmacist to report to the physician monitoring the pharmacist’s exercise of delegated drug therapy management and the results of the drug therapy management.
- A standard protocol may be used, or the attending physician may develop a drug therapy management protocol for the individual patient. If a standard protocol is used, the physician shall record, what deviations if any, from the standard protocol are ordered for that patient [22 TAC §193.15(e)].
The protocol under which a pharmacist initiates DTM orders for a patient should be available to the nurse at the facility, agency, or organization in which it is carried out. As with any order, the nurse must seek clarification if he/she believes the order is inappropriate, inaccurate, non-efficacious, or contraindicated by contacting the pharmacist and/or the physician who authorized the DTM protocol as appropriate [22 TAC §217.11(1)(N)]. The nurse carrying out an order for DTM written by a pharmacist is responsible and accountable for his/her actions just as he/she would be with any physician order.
(Board Action 01/2002; Revised: 01/2005; 01/2006; 01/2007; 01/2011; 01/2014; 01/2017; 01/2018; 01/2020)
(Reviewed: 01/2008; 01/2009; 01/2010; 01/2012; 01/2013; 01/2015; 01/2016; 01/2019; 01/2021)
Return to top
|
|
|
|
The Texas Board of Nursing (BON) has approved this position statement, only applicable to long term care settings, in an effort to provide guidance to registered nurses (RNs) in long-term care facilities and to clarify issues of compassionate end-of-life care. In 2002, The Texas Nurses Association (TNA) through its Long Term Care (LTC) Committee identified that RNs were concerned about the inappropriate initiation of cardiopulmonary resuscitation (CPR) when a resident without a "do-not-resuscitate" order (DNR) experiences unwitnessed arrest. There is a growing sentiment on the part of the long-term care nurse community that the initiation of CPR would appear futile and inappropriate given the nursing assessment of the resident.
The nursing community generally considers that initiation of CPR in such cases is not compassionate, and is not consistent with standards requiring the use of a systematic approach to provide individualized, goal directed nursing care [BON Standards of Nursing Practice, 22 TAC §217.11(3)]. This position statement is intended to provide guidance for RNs in the management of an unwitnessed resident arrest without a DNR order in a long-term care (LTC) setting. This position statement also addresses the related issues of:
- Obligation (or duty) of the RN to the resident;
- Expectation of supportive policies and procedures in LTC facilities; and
- The RN role in pronouncement of death.
These related issues are addressed in this position statement because the BON is often required to investigate cases of death where it appears there is a lack of clarity about a RN's obligation when there is no DNR order. The BON will evaluate cases involving the failure of a RN to initiate CPR in the absence of a DNR based on the following premise:
A DNR is a medical order that must be given by a physician and in the absence thereof, it is generally outside the standard of nursing practice to determine that CPR will not be initiated.
However, there may be instances when LTC residents without a DNR order experience an unwitnessed arrest, and it is clear according to the comprehensive nursing assessment that CPR intervention would be a futile and inappropriate intervention given the condition of the resident. In the case of an unwitnessed resident arrest without DNR orders, determination of the appropriateness of CPR initiation should be undertaken by the RN through an assessment of the resident, and interventions appropriate to the findings should be initiated.
Assessment of death in which CPR would be a futile and inappropriate intervention requires that all seven of the following signs be present and that the arrest is unwitnessed:
Presumptive Signs of Death
- The resident is unresponsive;
- The resident has no respirations;
- The resident has no pulse;
- The resident's pupils are fixed and dilated;
- The resident's body temperature indicates hypothermia: skin is cold relative to the resident’s baseline skin temperature;
- The resident has generalized cyanosis; and
Conclusive Sign of Death
- There is presence of livor mortis (venous pooling of blood in dependent body parts causing purple discoloration of the skin).
There may be other circumstances and assessment findings that could influence a decision on the part of the RN not to initiate CPR. However, evaluation of the prudence of such a decision would occur on a case-by-case basis by the BON.
Documentation
After assessment of the resident is completed and appropriate interventions are taken, documentation of the circumstances and the assessment of the resident in the resident's medical record is required. The rules of the BON establish legal documentation standards, [BON Standards of Nursing Practice, 22 TAC §217.11 (1)(D)]. Examples of important documentation elements include:
- Description of the discovery of the resident
- Any treatment of the resident that was undertaken
- The findings for each of the assessment elements outlined in the standards
- All individuals notified of the resident's status (e.g., 9-1-1, the health care provider, the administrator of the facility, family, coroner, etc.)
- Any directions that were provided to staff or others during the assessment and/or treatment of the resident
- The results of any communications
- Presence or absence of witnesses
Documentation should be adequate to give a clear picture of the situation and all of the actions that were taken or not taken on behalf of the resident.
Even if the RN's decision not to initiate CPR was appropriate, failure to accurately and completely document can result in an action against a nurse's license by the BON. Furthermore, lack of documentation places the nurse at a disadvantage should the nurse be required to explain the circumstances of the resident's death. RNs should be aware that actions documented at the time of death provide a more credible and accurate clinical description. Documentation that is absent, incomplete or inaccurate reveals gaps in care, requiring the nurse to prove actions not appropriately documented were actually taken. As stated in Position Statement 15.2, The Role of the Licensed Vocational Nurse in the Pronouncement of Death, it is beyond the scope of practice of the LVN to legally determine death, diagnose death, or otherwise pronounce death in the State of Texas. Therefore, the LVN cannot make a determination to withhold CPR.
Obligation (“Duty”) of the Nurse to the Resident
Whether CPR is initiated or not, it is important for the nurse to understand that the nurse may be held accountable if the nurse failed to meet standards of care to assure the safety of the resident, prior to the arrest such as:
- Failure to monitor the resident's physiologic status;
- Failure to document changes in the resident's status and to adjust the plan of care based on the resident assessment;
- Failure to implement appropriate interventions which might be required to stabilize a client's condition such as: reporting changes in the resident's status to the resident's primary care provider and obtaining appropriate orders; and/or
- Failure to implement procedures or protocols that could reasonably be expected to improve the resident's outcome.
Care Planning and Advanced Directives
Proactive policies and procedures, that acknowledge the importance of care planning with the inclusion of advanced directives, are also important. Evidence indicates that establishing the resident's wishes at the end of life and careful care planning prevents confusion on the part of nursing staff and assures that the resident's and family's wishes in all aspects of end of life care are properly managed.
The admission process to long-term care facilities in Texas requires that residents be provided information on self-determination and given the option to request that no resuscitation efforts be made in the event of cardiac and/or respiratory arrest. Facilities are required to have policies and adequate resources to assure that every resident and resident's family upon admission to a long term care facility not only receive such information, but have sufficient support to make an informed decision about end of life issues.
It is further expected that advanced care planning is an ongoing component of every resident's care and that the nursing staff should know the status of such planning for each resident.
The Board recognizes that end of life decisions on the part of residents and families can be difficult. However, the Board believes that principled and ethical discussion about CPR with the resident and family, is an essential element of the resident care plan.
RN Role in Pronouncement of Death
Texas law provides for RN pronouncement of death [Health & Safety Code §§ 671.001-.002]. The law requires that in order for an RN to pronounce death, the facility must have a written policy that is jointly developed and approved by the medical staff or medical consultant and the nursing staff specifying under what circumstances an RN can make a pronouncement of death.
It is important that nurses understand that the assessment that death has occurred and that CPR is not an appropriate intervention are not equivalent to the pronouncement of death. Texas statutory law governs who can pronounce death, and only someone legally authorized to pronounce death may do so. If the RN does not have the authority to pronounce death, upon assessment of death the RN must notify a person legally authorized to pronounce death.
Conclusion
This position statement is intended to guide RNs in long-term care facilities who encounter an unwitnessed resident arrest without a DNR order. It is hoped that by clarifying the responsibility of the RN, and using supportive facility policies and procedures, registered nurses will be better able to provide compassionate end of life care.
Qualifier to Position Statement
The BON evaluates "failure to initiate CPR cases" based on the premise that in the absence of a physician's DNR order it is generally outside the standard of nursing practice not to initiate CPR. Consequently, RNs who decide not to initiate CPR must assure themselves that not initiating CPR complies with their respective standards of practice, when their assessment determines that not all seven signs of death are present. Depending on the circumstances, a nurse's failure to initiate CPR when not all seven signs are present may constitute failure to comply with standards of nursing care. This position statement is limited to situations when all seven signs are present and should not be construed as providing guidance on the appropriateness of not initiating CPR when not all seven signs are present.
References
Texas Health and Safety Code §§ 671.001-671.002 https://statutes.capitol.texas.gov/Docs/HS/htm/HS.671.htm
American Heart Association. (2020). American Heart Association CPR&ECC guidelines. Retrieved from https://eccguidelines.heart.org/circulation/cpr-ecc-guidelines/
(Approved by the Board of Nursing on October 24, 2002; Revised: 01/2005; 01/2007; 01/2008; 01/2011; 01/2012; 01/2013; 01/2014; 01/2016; 01/2018; 01/2019; 01/2020; 01/2021)
(Reviewed: 01/2006; 01/2009; 01/2010; 01/2015; 01/2017)
Return to top
|
|
|
|
Advanced Practice Registered Nurses (APRN) often find themselves in situations where they may feel compelled to provide medical aspects of care or prescribe medications for themselves, their family members, or other individuals with whom they have a close personal relationship. APRNs are prohibited from ordering, prescribing or dispensing both medications and devices for personal use [22 TAC §222.10 (a) (2)]. When ordering, prescribing, or dispensing a medication or a device for any person, the APRN is expected to meet all standards of care including assessment, documentation of the assessment, diagnosis, and documentation of the plan of care prior to ordering, prescribing, dispensing, or administering a medication or device [22 TAC 222.10(a)(3)].
The practice of providing medical aspects of care for individuals with whom an APRN has a close personal relationship raises a number of ethical questions. The Board is concerned that APRNs in these situations risk allowing their personal feelings to cloud their professional judgment and objectivity. It is the opinion of the Board of Nursing that APRNs should not provide medical treatment or prescribe medications for any individual with whom they have a close personal relationship.
(Board Action 10/2003)
(Revised: 01/2009; 01/2014; 01/2018)
(Reviewed: 01/2006; 01/2007; 01/2008; 01/2010; 01/2011; 01/2012; 01/2013; 01/2015; 01/2016; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
Nursing is a dynamic profession. The scope of practice for one nurse may differ from the scope of practice for another nurse; therefore, it is impractical to create an exhaustive list of tasks that may or may not be performed by a nurse in any setting.
A number of complementary therapeutic modalities have long been incorporated into standard nursing practice to assist patients in meeting identified health needs and goals. Educational preparation to practice complementary modalities may be acquired through formal academic programs or continuing education.
Differentiating the Roles of the LVN and RN
The Licensed Vocational Nurse (LVN) and the professional or Registered Nurse (RN) have different roles within the nursing process. The nursing practice of an LVN requires supervision with oversight from an RN, advanced practice registered nurse, physician, physician assistant, podiatrist, or dentist. The LVN performs focused assessments and contributes to care planning, interventions, and evaluations. The RN is responsible for the overall coordination of care and performs comprehensive assessments, initiates the nursing care plan, and implements and evaluates care of the client or patient.
Additional references related to the topics of supervision, assessment, and the nursing process may be found in the following resources on the BON web site:
- Nursing Practice Act (NPA):
- 301.002, Definitions, and
- 301.353, Supervision of Vocational Nurse
- Board 22 TAC §217.11, Standards of Nursing Practice
- Position Statement 15.27, The Licensed Vocational Nurse Scope of Practice
- Frequently Asked Question: LVN's "Supervision of Practice"
- Frequently Asked Question: LVNs Performing Initial Assessments
Complementary Modalities
Depending upon the practice setting and modality considered, complementary modalities may be used alone or in conjunction with conventional modalities. Regardless of the practice setting, the LVN or RN who wishes to incorporate the use of complementary modalities into his/her nursing practice is accountable and responsible to adhere to the NPA and the Board Rules and Regulations Relating to Nursing Education, Licensure and Practice.
Rules that are particularly relevant to LVNs or RNs who integrate complementary therapies into nursing practice include 22 TAC §217.10, Restrictions to Use of Designations for Licensed Vocational or Registered Nurse, which requires a nurse who uses the title, either “LVN” or "RN" whether expressed or implied, to comply with the NPA and Board Rules. In addition, 22 TAC §217.11, Standards of Nursing Practice, forms the foundation for safe nursing practice and establishes the LVN’s or RN’s duty to his/her clients. While all standards apply when engaging in the practice of nursing, those standards most applicable to the nurse who engages in complementary modalities include 22 TAC §217.11(1)(A)-(D), (1)(F), (1)(G), (1)(R), and (1)(T). Additional standards may apply depending upon the specific practice situation. In order to show accountability when providing integrated or complementary modalities as nursing interventions, the LVN or RN should be able to articulate and provide evidence of:
- Educational activities used to gain or maintain the knowledge and skills needed for the safe and effective use of such modalities;
- Knowledge of the anticipated effects of the complementary therapy and its interactions with other modalities, including its physiological and/or emotional/spiritual impact;
- Selection of appropriate interventions, whether complementary, conventional, or in combination, to meet the client’s needs. The interventions and rationale for selection should be documented in the client’s nursing care plan. The demonstrated ability of the LVN or RN to properly perform the chosen intervention(s) should be maintained by the LVN or RN and/or his/her employer;
- Appropriate medical diagnosis and a valid order from a licensed provider as indicated.
- Instruction/education provided regarding the purpose of the selected intervention, e.g., how it is performed and its potential outcomes;
- Collaboration with other health care professionals and applicable referrals when necessary;
- Documentation of interventions and client responses in a client’s record;
- Development and/or maintenance of policies and procedures relative to complementary modalities when used in organized health care settings;
- Abstinence from making unsubstantiated claims about the therapy used; and
- Acknowledgment that, as with conventional modalities, each person’s response to the therapy will be unique.
While some complementary therapies, such as massage, have long been within the realm of nursing, there is a much broader connotation applied when an LVN or RN holds himself/herself out as a registered or certified practitioner of such a therapy. "Registered" or "certified" titles, in relation to a complementary modality, imply a degree of mastery above those basic skills acquired through a pre-licensure nursing program. The LVN or RN is accountable to hold the proper credentials (e.g., license, registration, certificate) to safely engage in the specific practice. Scope of Practice Decision-Making Model (DMM) (accessible on the Texas Board of Nursing (BON) web page) may be a useful tool for the LVN or RN who is uncertain whether a given modality is within his/her scope of practice. The nurse who wishes to integrate complementary modalities when engaging in the practice of nursing should be familiar with not only the NPA, BON rules, and any applicable Federal or State regulations, but also any prevailing standards published by national associations, credentialing bodies, and nursing organizations related to the LVN’s or RN’s area of practice.
(Board Action 01/2004)
(Revised: 01/2005; 01/2009; 04/2010; 01/2012; 01/2013; 01/2018; 01/2019)
(Reviewed: 01/2006; 01/2007; 01/2008; 01/2011; 01/2014; 01/2015; 01/2016; 01/2017; 01/2020; 01/2021)
Return to top
|
|
|
|
The Board of Nursing (Board or BON) approved curriculum for both licensed vocational nurses (LVNs) and registered nurses (RNs) does not provide graduates with sufficient instruction to provide the nurse with the necessary knowledge, skills and ability to re-insert and determine correct placement of a permanently placed feeding tube (such as gastrostomy or jejunostomy tubes). The Board does allow LVNs and RNs to expand their practice beyond the basic educational preparation through post-licensure continuing education and training for certain tasks and procedures. One of the main considerations in determining whether a nurse should consider re-insertion of a gastrostomy, jejunostomy or similar feeding tube, is how long the original tube was in place before becoming dislodged. Though sources vary, most give a range of 8-12 weeks for maturation/healing of the fistulous tract and stoma formation. The method of initial insertion (surgical, endoscopy, or radiographic guidance) may affect the length of healing. Orders should be obtained from the patient’s physician regarding re-insertion guidelines.
It is the opinion of the Board that LVNs and RNs should not engage in the reinsertion of a permanently placed feeding tube through an established tract until the LVN or RN successfully completes a competency validation course congruent with prevailing nursing practice standards. Training should provide instruction on the nursing knowledge and skills applicable to tube replacement and verification of correct and incorrect placement. The BON does not define nor set qualifications for competency validation courses; however, inclusion of the following factors is encouraged:
- The nurse should complete training designed specifically for the type or types of permanent feeding tubes the nurse may need to replace, including overall patient assessment, verification of proper tube placement, and assessment of the tube insertion site.
- A registered nurse or a physician who has the necessary expertise with regard to the specific feeding tube provides supervision during the training process.
- The nurse demonstrates competency in all appropriate aspects (knowledge, decision-making, and psychomotor skills) of performing the procedure.
- The patient has an established tract. The established tract is not determined by the nurse.
- The facility has resources available to develop an educational program for initial instruction of LVNs and/or RNs, as well as for ongoing competency validation.
- Documentation of each nurse’s initial education and ongoing competency validation should be maintained by the nurse and/or the employer in accordance with facility policies.
- Regardless of training, policies and procedures of the facility must also permit the nurse to engage in the procedure.
The nurse who accepts an assignment to engage in care and/or replacement of permanently placed feeding tubes is responsible to adhere to the NPA and Board rules, particularly 22 TAC §217.11, Standards of Nursing Practice, as well as any other standards or rules applicable to the nurse’s practice setting. Two standards applicable in all practice scenarios include:
- 22 TAC §217.11(1)(B) “implement measures to promote a safe environment for clients and others;” and
- 22 TAC §217.11(1)(T) “accept only those assignments that take into consideration client safety and that are commensurate with the nurse’s educational preparation, experience, knowledge, and physical and emotional ability.”
Additional standards in 22 TAC §217.11 that may be applicable when a nurse chooses to engage in replacement of a permanently placed feeding tube include (but are not limited to):
- (1)(D) “accurately and completely report and document: (i) ...client status...(ii) nursing care rendered; (iii) physician, dentist or podiatrist orders; (iv) administration of medications and treatments; (v) client response(s)...,”
- (1)(G) “obtain instruction and supervision as necessary when implementing nursing procedures or practices,”
- (1)(H) “make a reasonable effort to obtain orientation/training for competency when encountering new equipment and technology or unfamiliar care situations,”
- (1)(R) “be responsible for one’s own continuing competence in nursing practice and individual professional growth.”
- Standards specific to LVNs may be found in 22 TAC §217.11(2); standards specific to RNs may be found in 22 TAC §217.11(3).
Regardless of facility policy or physicians’ orders, the nurse always has a duty to maintain the safety of the patient [Reference 22 TAC §217.11(1)(B) above]; this standard has previously been upheld in a landmark case [Lunsford v. Board of Nurse Examiners, 648 S.W. 2d 391 (Tex. App. -- Austin 1983)].
(Adopted 01/2005)
(Revised: 01/2008; 01/2009; 01/2011; 01/2013; 01/2018)
(Reviewed: 01/2006; 01/2007; 01/2010; 01/2012; 01/2014; 01/2015; 01/2016; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
|
|
|
The definition of “Vocational Nursing” in the Texas Occupations Code states:
“Vocational Nursing” means a directed scope of nursing practice, including the performance of an act that requires specialized judgment and skill, the proper performance of which is based on knowledge and application of the principles of biological, physical, and social science as acquired by a completed course in an approved school of vocational nursing. The term does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures.
Vocational nursing involves:
- collecting data and performing focused nursing assessments of the health status of an individual;
- participating in the planning of the nursing care needs of an individual;
- participating in the development and modification of the nursing care plan;
- participating in health teaching and counseling to promote, attain, and maintain the optimum health level of an individual;
- assisting in the evaluation of an individual’s response to a nursing intervention and the identification of an individual’s needs; and
- engaging in other acts that require education and training, as prescribed by board rules and policies, commensurate with the nurse’s experience, continuing education, and demonstrated competency [TOC 301.002(5)].
Educational preparation leading to initial licensure as a nurse in Texas is described in the Differentiated Essential Competencies of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors (DECs)(Oct 2010). This document lists the minimum competency expectations for graduates of Vocational (VN), Diploma/Associate Degree (Diploma/ADN), and Baccalaureate Degree (BSN) nursing programs. According to the DECs, educational preparation for Vocational Nurses includes the following related to administration of medications:
Knowledge:
- Common medical diagnoses, drug and other therapies and treatments.
Clinical Behavior/Judgments:
- Administer medications and treatments and perform procedures safely, and
- Monitor, document, and report responses to medications, treatments, and procedures and communicate the same to other health care professionals clearly and accurately.
The Standards of Nursing Practice (22 TAC §217.11) applicable to LVNs (as well as RNs) includes the following standards that specifically relate to medication administration:
- (1)(C) Know the rationale for and effects of medications and treatments, and shall correctly administer the same;
- (1)(D) Accurately and completely report and document: (iv) administration of medications and treatments;
- (1)(N) Clarify any order or treatment regimen that the nurse has reason to believe is inaccurate, non-efficacious or contraindicated by consulting with the appropriate licensed practitioner and notifying the ordering practitioner when the nurse makes the decision not to administer the medication or treatment.
[Note that other standards may apply to administration of medications within a given practice circumstance.]
The Board’s position, therefore, is that LVNs are educationally prepared to administer medications and treatments as ordered by a physician, podiatrist, dentist, or any other practitioner legally authorized to prescribe the ordered medication. LVNs may also administer medications and treatments ordered by PAs and APRNs as established under Position Statements 15.1 and 15.18, relating to nurses accepting orders from Physician Assistants (PAs) and Advanced Practice Registered Nurses (APRNs), respectively.
Each LVN has different experiences, knowledge, level of competence, and abilities; therefore, it is up to the individual LVN to use sound judgment when determining the individual
LVN’s scope of practice. The following documents on the Board’s web page may be helpful for a LVN concerned about his/her scope of practice for administration of medications or other nursing practice concerns:
(Adopted 10/2005)
(Revised: 01/2009; 01/2011; 01/2012; 01/2013; 01/2016; 01/2018)
(Reviewed: 01/2007; 01/2008; 01/2010; 01/2014; 01/2015; 01/2017; 01/2019; 01/2020; 01/2021)
Return to top
|
15.27 The Licensed Vocational Nurse Scope of Practice
|
|
The BON recommends that all nurses utilize the Scope of Practice Decision-Making Model (DMM) 1 when deciding if an employer’s assignment is safe and legally within the nurse’s scope of practice.
The Texas Board of Nursing (BON or Board) is authorized by the Texas Legislature to regulate the nursing profession to ensure that every licensee is competent to practice safely. The Texas Nursing Practice Act (NPA) and the Board’s Rules and Regulations define the legal scope of practice for licensed vocational nurses (LVN). The LVN scope of practice is a directed scope of practice and requires appropriate supervision. The LVN, with a focus on patient safety, is required to function within the parameters of the legal scope of practice and in accordance with the federal, state, and local laws, rules, and regulations. In addition, the LVN must comply with policies, procedures and guidelines of the employing health care institution or practice setting. The LVN is responsible for providing safe, compassionate and focused nursing care to assigned patients with predictable health care needs.
The purpose of this position statement is to provide direction and recommendations for nurses and their employers regarding the safe and legal scope of practice for LVNs and to promote an understanding of the differences between the LVN and registered nurse (RN) levels of licensure. The RN scope of practice is interpreted in Position Statement 15.28.
Every nursing education program in the state of Texas is required to ensure that their graduates exhibit competencies outlined in the Board’s Differentiated Essential Competencies of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors (DECs)(Oct 2010)2. These competencies are included in the program of study so that every graduate has the knowledge, clinical judgment and behaviors necessary for LVN entry into safe, competent and compassionate nursing care. The DECs serve as a guideline for employers to assist LVNs as they transition from the educational environment into nursing practice. As LVNs enter the workplace, the DECs serve as the foundation for the development of the LVN scope of practice.
Completion of on-going, informal continuing nursing education offerings and on-the-job trainings in an LVN’s area of practice serves to develop, maintain, and expand the level of competency. Because the LVN scope of practice is based upon the educational preparation in the LVN program of study, there are limits and parameters to LVN scope of practice expansion. The Board believes that for a nurse to successfully make a transition from one level of nursing practice to another requires the nurse to complete a formal education program.3
The LVN Scope of Practice
The LVN is an advocate for the patient and the patient’s family and promotes safety by practicing in accordance with the NPA and the BON Rules and Regulations. LVN scope of practice does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures.4 The practice of vocational nursing must be performed under the supervision of a RN, advanced practice registered nurse (APRN), physician, physician assistant, podiatrist or dentist.5 Supervision is defined as the process of directing, guiding, and influencing the outcome of an individual’s performance of an activity.6 The LVN is precluded from practicing in a completely independent manner; however, direct and on-site supervision may not be required in all settings or patient care situations. Determining the proximity of an appropriate clinical supervisor, whether available by phone or physical presence, should be made by the LVN and the LVN’s clinical supervisor by evaluating the specific situation, taking into consideration patient conditions and the level of skill, training and competence of the LVN. An appropriate clinical supervisor may need to be physically available to assist the LVN should emergent situations arise.
The setting in which the LVN provides nursing care should have well defined policies, procedures, and guidelines, in which assistance and support are available from an appropriate clinical supervisor. The Board recommends that newly licensed LVNs work in structured settings for a period of 12-18 months, such as nursing homes, hospitals, rehabilitation centers, skilled nursing facilities, clinics or private physician offices.7 This allows the new nurse sufficient practice experience in more structured settings in order to assimilate knowledge from their education. As competencies are demonstrated, if the LVN transitions to unstructured settings where the clinical supervisor may not be on-site, it is the LVN’s responsibility to ensure he or she has access to an appropriate clinical supervisor and that the policies, procedures and guidelines for that particular setting are established to guide LVN practice.
The LVN uses a systematic problem-solving process in the care of multiple patients with predictable health care needs to provide individualized, goal-directed nursing care. LVNs may contribute to the plan of care by collaborating with interdisciplinary team members, the patient and the patient’s family. The essential components of the nursing process are described in a side-by-side comparison of the different levels of education and licensure (see Table).
Assessment
The LVN assists in determining the physical and mental health status, needs, and preferences of culturally, ethnically, and socially diverse patients and their families based on interpretation of health-related data. The LVN collects data and information, recognizes changes in conditions and reports this to the RN supervisor or another appropriate clinical supervisor to assist in the identification of problems and formulation of goals, outcomes and patient-centered plans of care that are developed in collaboration with patients, their families, and the interdisciplinary health care team. The LVN cannot perform independent assessments as the LVN has a directed scope of practice under supervision. The LVN participates in the nursing process by appraising the individual patient’s status or situation at hand. Also known as a focused assessment, this appraisal may be considered a component of a more comprehensive assessment performed by a RN or another appropriate clinical supervisor. For example, a RN may utilize the data and information collected and reported by the LVN in the formation of the nursing plan of care; however, the RN’s comprehensive assessment lays the foundation for the nursing process. The LVN reports the data and information collected either verbally or in writing. The LVN must also document this data and information, the written documentation must be accurate and complete, and according to policies, procedures and guidelines for the employment setting.
Nursing Diagnosis/Problem Identification/Planning
The second step in the nursing process is nursing diagnosis or the identification of problems. The role of the LVN is to report data to assist in the identification of problems and formulation of goals/outcomes and patient-centered plans of care in collaboration with patients, their families, and the interdisciplinary health care team.
The third step in the nursing process in which the LVN participates and contributes to the nursing process is planning nursing care needs of patients. After the focused assessment, the LVN reports data and other information such as changes in patient conditions to the appropriate clinical supervisor, such as an RN. This information may be considered in planning, problem identification, nursing diagnoses, and formulation of goals, teaching plans, and outcomes by the RN supervisor or another appropriate clinical supervisor. A nursing plan of care for patients is developed by the RN and thus the RN has the overall responsibility to coordinate nursing care for patients; however the LVN participates in the development and modification of the nursing care plan.
Implementation
Implementing the plan of care is the fourth step in the nursing process. The LVN is responsible for providing safe, compassionate and focused nursing care to assigned patients with predictable health care needs. The LVN may implement aspects of the plan of care within legal, ethical, and regulatory parameters and in consideration of patient factors. The LVN organizes aspects of patient care based on identified priorities. Delegating tasks to unlicensed assistive personnel (UAPs) is beyond the scope of practice for LVNs; however, LVNs may make appropriate assignments to other LVNs and UAPs according to Rule 217.11(2).6 The RN is generally responsible and accountable for supervising not only the LVN's practice but the UAP’s performance of tasks as well. For example, the RN may have trained, verified competency and delegated the tasks to a UAP and the LVN may then proceed to assign those tasks that need to be accomplished for that day. Teaching and counseling are interwoven throughout the implementation phase of the nursing process and LVNs can participate in implementing established teaching plans for patients and their families with common health problems and well defined health learning needs.
Evaluation
A critical and final step in the nursing process is evaluation. The LVN participates in the evaluation process by identifying and reporting any alterations in patient responses to therapeutic interventions in comparison to expected outcomes. The LVN may contribute to the evaluation phase by suggesting any modifications to the plan of care that may be necessary and making appropriate referrals to facilitate continuity of care.
Essential Skills Used in the Nursing Process
Communication
Communication is a fundamental component in the nursing process. The LVN must communicate verbally, in writing, or electronically with members of the healthcare team, patients and their families on all aspects of the nursing care provided to patients. Communications must be appropriately documented in the patient record or nursing care plan. Because LVNs are members of the healthcare team, provide nursing care, and contribute to the nursing process, collaboration is crucial to the communication process. When patient conditions or situations have changed or exceeded the LVN’s level of competency and scope of practice, the LVN must be prepared to seek out his or her clinical supervisor and actively communicate and collaborate to develop solutions that ensure patient safety.
Clinical Reasoning
Clinical reasoning is another integral component in the nursing process. LVNs must use clinical reasoning and established evidence-based policies, procedures, or guidelines as the basis for decision making in nursing practice. LVNs are accountable and responsible for the quality of nursing care provided and must exercise prudent nursing judgment to ensure the standards of nursing practice are met at all times.
Employment Setting
When an employer hires a nurse to perform a job, the nurse must assure that it is safe and legal. For instance, the LVN must have a clinical supervisor who is knowledgeable and aware of his or her role. Caution must be exercised not to overstep the legal parameters of nursing practice when an employer may not understand the limits of the LVN scope of practice and makes an assignment that is not prudent or safe. The LVN must determine before he or she engages in an activity or assignment whether he or she has the education, training, skill, competency, and the physical and emotional ability to safely carry out the activity or assignment. The LVN’s duty is to always provide safe, compassionate, and focused nursing care to patients.
Making Assignments
The LVN’s duty to patient safety when making assignments to others is to take into consideration the education, training, skill, competence, and physical and emotional ability of the persons to whom the assignments are made.
If the LVN makes assignments to another LVN or UAP, he or she is responsible for reasonable and prudent decisions regarding those assignments. It is not appropriate and is beyond the scope of practice for an LVN to supervise the nursing practice of an RN. However, in certain settings, i.e., nursing homes, LVNs may expand their scope of practice through experience, skill, and continuing education to include supervising the practice of other LVNs, under the oversight of an RN or another appropriate clinical supervisor. The supervising LVN may have to directly observe and evaluate the nursing care provided depending on the LVN’s skills and competence, patient conditions and level of urgency in emergent situations. Timely and readily available communication between the supervising LVN and the clinical supervisor is essential to provide safe and effective nursing care.
Summary
The LVN, with a focus on patient safety, is required to function within the parameters of the legal scope of practice and in accordance with the federal, state, and local laws, rules, regulations, and policies, procedures and guidelines of the employing health care institution or practice setting. The LVN functions under his or her own license and assumes accountability and responsibility for the quality of care provided to patients and their families according to the standards of nursing practice. The LVN demonstrates responsibility for continued competence in nursing practice, and develops insight through reflection, self-analysis, self-care, and lifelong learning.
The table below offers a brief synopsis of how the scope of practice for nurses differs based on educational preparation and level of licensure. These are minimum competencies, but also set limits on what the LVN or RN can do at his or her given level of licensure, regardless of experience.
15.27 - Table (Synopsis of Differences in Scope of Practice)
Scope of Practice for Nurses - Poster
Resources
1 Texas Board of Nursing (2019). Scope of Practice Decision-Making Model (DMM).
2 Texas Board of Nursing (2010). Differentiated essential competencies of graduates of Texas Nursing Programs evidenced by knowledge, clinical judgements, and behaviors (DECs).
3 Texas Board of Nursing (2015). Position statement 15.10, Continuing education: Limitations for expanding scope of practice.
4 Texas Nursing Practice Act, TOC § 301.002(5).
5 Texas Nursing Practice Act, TOC § 301.353.
6 22 TAC §217.11(2).
7 Texas Board of Nursing (2015). Rules and guidelines governing the graduate vocational and registered nurse candidates or newly licensed vocational or registered nurse.
8 22 TAC §217.11(1).
(Adopted: 07/2011; Revised: 01/2013; 01/2016; 01/2018; 01/2019; 01/2020)
(Reviewed: 01/2012; 01/2014; 01/2015; 01/2017; 01/2021)
Return to top
|
15.28 The Registered Nurse Scope of Practice
|
|
The BON recommends that all nurses utilize the Scope of Practice Decision-Making Model (DMM) 1 when deciding if an employer’s assignment is safe and legally within the nurse’s scope of practice.
The Texas Board of Nursing (BON or Board) is authorized by the Texas Legislature to regulate the nursing profession to ensure that every licensee is competent to practice safely. The Texas Nursing Practice Act (NPA) defines the legal scope of practice for professional registered nurses (RN).2 The RN takes responsibility and accepts accountability for practicing within the legal scope of practice, is prepared to work in all health care settings, and may engage in independent nursing practice without supervision by another health care provider. The RN, with a focus on patient safety, is required to function within the parameters of the legal scope of practice and in accordance with the federal, state, and local laws, rules and regulations. In addition, the RN must comply with policies, procedures and guidelines of the employing health care institution or practice setting. The RN is responsible for providing safe, compassionate, and comprehensive nursing care to patients and their families with complex healthcare needs.
The purpose of this position statement is to provide direction and recommendations for nurses and their employers regarding the safe and legal scope of practice for RNs and to promote an understanding of the differences in the RN programs of study and between the RN and LVN levels of licensure. The LVN scope of practice is interpreted in Position Statement 15.27.
Every nursing education program in the state of Texas is required to ensure that their graduates exhibit competencies outlined in the Board’s Differentiated Essential Competencies of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors (DECs)(Oct 2010)3. These competencies are included in the program of study so that every graduate has the knowledge, clinical judgment and behaviors necessary for RN entry into safe, competent, and compassionate nursing care. The DECs serve as a guideline for employers to assist RNs as they transition from the educational environment into nursing practice. As RNs enter the workplace, the DECs serve as the foundation for the development of the RN scope of practice.
Completion of on-going, informal continuing nursing education offerings and on-the-job trainings in a RN’s area of practice serves to develop, maintain, and expand competency. Because the RN scope of practice is based upon the educational preparation in the RN program of study, there are limits to the expansion of the scope. The Board believes that for a nurse to successfully make a transition from one level of nursing practice to another requires the nurse to complete a formal education program.4
The RN Scope of Practice
The professional RN is an advocate for the patient and the patient’s family, and promotes safety by practicing within the NPA and the BON Rules and Regulations. The RN provides nursing services that require substantial specialized judgment and skill. The planning and delivery of professional nursing care is based on knowledge and application of the principles of biological, physical, and social science as acquired by a completed course of study in an approved school of professional nursing. Unless licensed as an advanced practice registered nurse, the RN scope of practice does not include acts of medical diagnosis or the prescription of therapeutic or corrective measures.2 RNs utilize the nursing process to establish the plan of care in which nursing services are delivered to patients. The level and impact of the nursing process differs between the RN and LVN as well as between the different levels of RN education (see Table).
Assessment
The comprehensive assessment is the first step, and lays the foundation for the nursing process. The comprehensive assessment is the initial and ongoing, extensive collection, analysis and interpretation of data. Nursing judgment is based on the assessment findings. The RN uses clinical reasoning and knowledge, evidence- based outcomes, and research as the basis for decision-making and comprehensive care. Based upon the comprehensive assessment the RN determines the physical and mental health status, needs, and preferences of culturally, ethnically, and socially diverse patients and their families using evidence-based health data and a synthesis of knowledge. Surveillance is an essential step in the comprehensive assessment process. The RN must anticipate and recognize changes in patient conditions and determines when reassessments are needed.
Nursing Diagnosis/Problem Identification/Planning
The second step in the nursing process is nursing diagnosis and problem identification. The role of the RN is to synthesize comprehensive assessment data to identify problems, formulate goals/outcomes, and develop plans of care for patients, families, populations, and communities using information from evidence-based practice and published research in collaboration with these groups and the interdisciplinary health care team.
The third step in the nursing process is planning. The RN synthesizes the data collected during the comprehensive assessment to identify problems, make nursing diagnoses, and to formulate goals, teaching plans and outcomes. A nursing plan of care for patients is developed by the RN, who has the overall responsibility to coordinate nursing care for patients. Teaching plans address health promotion, maintenance, restoration, and prevention of risk factors. The RN utilizes evidence-based practice, published research, and information from patients and the interdisciplinary health care team during the planning process.
Implementation
Implementing the plan of care is the fourth step in the nursing process. The RN may begin, deliver, assign, or delegate certain interventions within the plan of care for patients within legal, ethical, and regulatory parameters and in consideration of health restoration, disease prevention, wellness, and promotion of healthy lifestyles. The RN’s duty to patient safety when making assignments to other nurses or when delegating tasks to unlicensed staff is to consider the education, training, skill, competence, and physical and emotional abilities of those to whom the assignments or delegation is made. The RN is responsible for reasonable and prudent decisions regarding assignments and delegation. The RN scope of practice may include the supervision of LVNs or other RNs. Supervision of LVN staff is defined as the process of directing, guiding, and influencing the outcome of an individual’s performance and activity.5 The RN may have to directly observe and evaluate the nursing care provided depending on the LVN’s skills and competence, patient conditions, and level of urgency in emergent situations.
The RN may determine when it is appropriate to delegate tasks to unlicensed personnel and maintains accountability for how the unlicensed personnel perform the tasks. The RN is responsible for supervising the unlicensed personnel when tasks are delegated. The proximity of supervision is dependent upon patient conditions and skill level of the unlicensed personnel. In addition, teaching and counseling are interwoven throughout the implementation phase of the nursing process.
Evaluation and Re-assessment
A critical and final step in the nursing process is evaluation. The RN evaluates and reports patient outcomes and responses to therapeutic interventions in comparison to benchmarks from evidence-based practice and research findings, and plans any follow-up care and referrals to appropriate resources that may be needed. The evaluation phase is one of the times when the RN reassesses patient conditions and determines if interventions were effective and if any modifications to the plan of care are necessary.
Essential Skills Used in the Nursing Process
Communication
Communication is an essential and fundamental component used during the nursing process. The RN must communicate verbally, in writing, or electronically with members of the healthcare team, patients and their families in all aspects of the nursing care provided to patients. These communications must be appropriately documented in the patient record or nursing care plan. Because RNs plan, coordinate, initiate and implement a multidisciplinary team’s approach to patient care, collaboration is crucial to the communication process. When patient conditions or situations exceed the RN’s level of competency, the RN must be prepared to seek out other RNs with greater competency or other health care providers with differing knowledge and skill sets and actively cooperate to ensure patient safety.
Clinical Reasoning
Clinical reasoning is another integral component in the nursing process. RNs use critical thinking skills to problem-solve and make decisions in response to patients, their families and the healthcare environment. RNs are accountable and responsible for the quality of nursing care provided and must exercise prudent and professional nursing judgment to ensure the standards of nursing practice are met at all times.
Employment Setting
When an employer hires an RN to perform a job, the RN must assure that it is safe and legal. Caution must be exercised not to overstep the legal parameters of nursing practice when an employer may not understand the limits of the RN scope of practice and makes an assignment that is not safe. The RN must determine before he or she engages in an activity or assignment whether he or she has the education, training, skill, competency and the physical and emotional ability to safely carry out the activity or assignment. The RN’s duty is to always provide safe, compassionate, and comprehensive nursing care to patients.
Summary
The RN, with a focus on patient safety, is required to function within the parameters of the legal scope of practice and in accordance with the federal, state, and local laws; rules and regulations; and policies, procedures and guidelines of the employing health care institution or practice setting. The RN functions under his or her own license and assumes accountability and responsibility for quality of care provided to patients and their families according to the standards of nursing practice. The RN demonstrates responsibility for continued competence in nursing practice, and develops insight through reflection, self-analysis, self-care, and lifelong learning.
The table below offers a brief synopsis of how the scope of practice for nurses differs based on educational preparation and level of licensure. These are minimum competencies, but also set limits on what the LVN or RN can do at his or her given level of licensure, regardless of experience.
15.28 - Table (Synopsis of Differences in Scope of Practice)
Scope of Practice for Nurses - Poster
Resources
1 Texas Board of Nursing (2019). Scope of Practice Decision-Making Model (DMM).
2 Nursing Practice Act, TOC §301.002(2)
3 Texas Board of Nursing (2010). Differentiated Essential Competencies of Graduates of Texas Nursing Programs Evidenced by Knowledge, Clinical Judgements, and Behaviors (DECs).
4 Texas Board of Nursing (2017). Position statement 15.10, Continuing education: Limitations for expanding scope of practice.
5 22 TAC §217.11(2)
(Adopted: 07/2011; Revised: 01/2013; 01/2016; 01/2018; 01/2019; 01/2020)
(Reviewed: 01/2012; 01/2014; 01/2015; 01/2017; 01/2021)
Return to top
|
15.29 Professional Boundaries including Use of Social Media by Nurses
|
|
The purpose of this Position Statement is to provide guidance to nurses regarding expectations related to professional boundaries, inclusive of social media, and to provide nurses with guidance to prevent boundary violations.
The Texas Board of Nursing (BON or Board), in keeping with its mission to protect the public health, safety, and welfare, holds nurses accountable for knowing, recognizing, and maintaining professional boundaries of the nurse-patient/client relationship [22 TAC §217.11 (1)(J)]. The term professional boundaries is defined as: the appropriate limits which should be established by the nurse in the nurse/client relationship due to the nurse's power and the patient's vulnerability. Professional boundaries refers to the provision of nursing services within the limits of the nurse/client relationship which promote the client's dignity, independence and best interests and refrain from inappropriate involvement in the client's personal relationships and/or the obtainment of the nurse's personal gain at the client's expense [22 TAC §217.1(29)].
The National Council of State Boards of Nursing (NCSBN) defines professional boundaries as the spaces between the nurse's power and the patient's vulnerability. The power of the nurse comes from the nurse's professional position and access to sensitive personal information. The difference in personal information the nurse knows about the patient versus personal information the patient knows about the nurse creates an imbalance in the nurse-patient relationship. Nurses should make every effort to respect the power imbalance and ensure a patient-centered relationship.
Common to the definition of professional boundaries from the Texas Board of Nursing and from the NCSBN is that a nurse abstains from personal gain at the client's expense and the nurse refrains from inappropriate involvement with the patient or the patient's family.
Duty of a Nurse in Maintenance of Professional Boundaries
There is a power differential between the nurse and the patient. The patient depends on the knowledge of the nurse and relies on the nurse to advocate for the patient and to ensure actions are taken in the patient's best interest. The nurse has a duty to protect the patient including establishing and maintaining professional boundaries in the nurse-patient/client relationship. Under or over involvement can be harmful to the patient and may interfere with the nurse-patient relationship. Visualizing the two ends of the spectrum may assist the nurse in knowing, recognizing and maintaining the professional boundaries of nurse-patient relationships.
Patients each have their own unique needs and abilities. The boundary line for any one particular patient may change over time and may not be the same as the boundary line for another patient. It is up to the nurse to assess the patient and recognize the patient’s needs, adjusting the nursing care accordingly. Every nurse is responsible for knowing, recognizing, and maintaining the professional boundaries of the nurse-client relationship [§217.11(1)(J)].
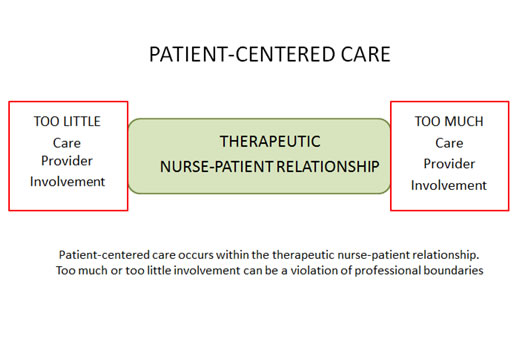
Boundary Violations
A violation of professional boundaries is one element of the definition of "conduct subject to reporting [Tex. Occ. Code Sec. 301.401(1)(C)]. A professional boundary violation is also considered unprofessional conduct [22 TAC §217.12 (6)(D)]. Some of the specific categories of professional boundary violations include, but are not limited to physical, sexual, emotional, or financial boundary violations.
Use of Social Media
The use of social media and other electronic communication is expanding exponentially as the number of social media outlets, platforms and applications available continue to increase. Nurses play a significant role in the identification, interpretation, and transmission of knowledge and information within healthcare. As technological advances continue to expand connectivity and communication, rapid knowledge exchange and dissemination can pose risks to both patients and nurses. While the Board recognizes that the use of social media can be a valuable tool in healthcare, there are potentially serious consequences if used inappropriately. A nurse's use of social media may cause the nurse to unintentionally blur the lines between the nurse's professional and personal life.
Online postings may harm patients if protected health information is disclosed. In addition, social media postings may reflect negatively on individual nurses, the nursing profession, the public's trust of the nursing profession, or the employer and may jeopardize careers. In a survey by the NCSBN, many of the responding boards reported that they had received complaints about nurses inappropriately using social media sites. The survey results indicated that nurses have been disciplined by boards, fired by employers, and criminally charged for the inappropriate or unprofessional use of social media (NCSBN, 2012).
To ensure the mission to protect and promote the welfare of the people of Texas, the Texas Board of Nursing supports both the guidelines and principles of social media use by the NCSBN and American Nurses Association. In accordance with the NCSBN guidelines and Board rules, it is the Board's position that:
- Nurses have an ethical and legal obligation to maintain patient privacy and confidentiality at all times. When using social media, nurses do not identify patients by name or post or publish information that may lead to the identification of a patient. Limiting access to postings through privacy settings is not sufficient to ensure privacy. Nurses must promptly report any identified breach of confidentiality or privacy [Board Rule 217.11(1) (E) and (K)].
- Nurses maintain professional boundaries in the use of electronic media. The nurse has the obligation to establish, communicate and enforce professional boundaries with patients in the online environment. Nurses do not refer to patients in a disparaging manner, even if the patient is not identified or transmit information that may be reasonably anticipated to violate patient rights to confidentiality or privacy, or otherwise degrade or embarrass the patient [Board Rule 217.11(1) (J)].
- Nurses must provide nursing services without discrimination and do not make threatening, harassing, profane, obscene, sexually explicit, racially derogatory, homophobic or other offensive comments [Board Rules 217.11(1) (L) and 217.12 (6)(C), (D), and (F)].
- Nurses must be aware of and comply with all laws and rules, including employer policies regarding the use of electronic devices including employer-owned computers, cameras and use of personal devices in the work place. In addition, nurses must ensure appropriate and therapeutic use of all patient-related electronic media, including patient-related images, photos, or videos in accordance with applicable laws, rules, and institutional policies and procedures [Board Rule 217.11(1)(A)].
The use of social media can be of tremendous benefit to nurses and patients alike, for example dissemination of public safety announcements. However, nurses must be aware of the potential consequences of disclosing patient-related information via social media. Nurses must always maintain professional standards, boundaries, and compliance with local, state, and federal laws as stated in 22 TAC §217.11(1)(A). All nurses have an obligation to protect their patient’s privacy and confidentiality (as required by 22 TAC §217.11(1)(E) which extends to all environments, including the social media environment.
Resources
American Nurses Association. (n.d.). Social Media. Retrived from https://www.nursingworld.org/social/
American Nurses Association. (2017). Social networking privacy toolkit. Retrieved from https://www.nursingworld.org/practice-policy/nursing-excellence/social-networking-Principles
National Council of State Boards of Nursing. (2014). A nurse’s guide to professional boundaries. Retrieved from https://www.ncsbn.org/ProfessionalBoundaries_Complete.pdf
National Council of State Boards of Nursing. (2014). Social media guidelines for nurses. Retrieved from https://www.ncsbn.org/347.htm
National Council of State Boards of Nursing. (2011). White Paper: A nurse’s guide to the use of social media. Chicago, IL
22 TAC §217.1(29) (2016).
22 TAC §217.11(1)(J) (2016).
(Adopted: 04/2012)
(Revised: 01/2013; 01/2014; 01/2017; 01/2018; 01/2019; 01/2021)
(Reviewed: 01/2015; 01/2016; 01/2020)
Return to top
|
|
|
The mission of the Texas Board of Nursing (Board or BON) is to protect and promote the welfare of the people of Texas by ensuring that each person holding a license as a nurse in the State of Texas is competent to practice safely. To provide further guidance for nurses on relevant practice and licensure issues the Board develops position statements, however they do not have the force of law. This position statement addresses an issue facing nursing practice today, workplace violence.
Violence in the workplace, including bullying, affects both patients and nurses, and can disrupt communication and teamwork, interfering with the nurse’s ability to promote a safe patient care environment. The American Nurses Association attests that “evidence-based best practices must be implemented to prevent and mitigate incivility, bullying, and workplace violence” to support the safety of nurses and safeguard optimal patient outcomes.1 It is important for nurses to maintain professionalism, through communication, conduct, and caring behaviors. The Board believes that professional behaviors that are in alignment with Board Rule 217.11- Standards of Nursing Practice can assist nurses in eliminating workplace violence.
Violence in the Workplace
The Occupational Safety and Health Administration (OSHA) defines workplace violence to include "any act or threat of physical violence, harassment, intimidation, or other threatening disruptive behavior that occurs at the work site.”2 With healthcare and social service workers facing “a significant risk of job-related violence”3, in 2016, the Texas Center for Nursing Workforce Studies (TCNWS) conducted a statewide study on workplace violence against nurses. This study was performed in hospitals, freestanding emergency medical care facilities, nursing facilities, and home health agencies, as required by House Bill (HB) 2696, 84th Texas Legislature, Regular Session, 2015 which added Section 105.009 to the Health and Safety Code.4 The TCNWS Advisory Committee issued recommendations based on the study findings to:
- promote safer facilities,
- encourage nursing staffing committees to consider incidents of workplace violence,
- encourage reporting of violent events, and
- establish and maintain ongoing surveillance of workplace violence.
Based on these findings, workplace violence remained a priority during the 85th Texas Legislature, Regular Session, as HB 280 passed requiring the Board of Nursing, under Section 301.155, Occupations Code, to fund grant programs administered by the TCNWS for reducing workplace violence against nurses. HB 280 seeks to alleviate the trauma of workplace violence by providing grants to hospitals and other health facilities to implement innovative approaches unique to each facility and region to reduce the severity and frequency of these occurrences.
Collaborative Approach to Address Workplace Violence
Effective management of workplace violence begins by recognizing that workplace violence is a safety and health hazard. Nurses work with patients of differing backgrounds and in various practice settings at times when patients may experience “pain, devastating prognoses, unfamiliar surroundings, mind and mood altering medications and drugs, and disease progression” which can “cause agitation and violent behaviors.”3
The healthcare team must commit to work collaboratively in support of effective violence prevention programming. This commitment should include acknowledging the value of a safe, violence-free workplace, ensuring and exhibiting equal commitment to the safety and health of workers and patients/clients, while maintaining a system of accountability for all involved members of the health care team.
Nurses may provide expertise and useful information, collaborating to design, implement and evaluate workplace violence prevention programming.3
Standards of Nursing Practice Related to Workplace Violence
Consideration of and compliance with Board Rule 217.11-Standards of Nursing Practice is essential when providing care to a patient in a potentially violent situation. It is the Board’s position that:
- Nurses must be aware of and comply with all laws and rules, including employer policies, regarding workplace violence [Board Rule 217.11(1)(A)].
- Nurses implement measures to promote a safe environment for patients and others [Board Rule 217.11(1)(B)]. This would include the creation and implementation of policies, procedures, and interventions to mitigate and/or eliminate workplace violence in the interests of a safe patient care environment.
- Nurses respect the client’s right to privacy by protecting confidential information unless required or allowed by law to disclose the information [Board Rule 217.11(1)(E)]. Though acts of violence toward an individual can be a frightening and potentially dangerous situation, it is important to continue to respect the patient’s privacy, and withhold patient identifiers when disclosing information about the incident, unless disclosure is required by law or to prevent harm5.
- Nurses obtain instruction and supervision as necessary when implementing nursing procedures or practices, make a reasonable effort to obtain orientation/training for competency when encountering new equipment and technology or unfamiliar care situations, and maintain responsibility for individual professional growth and continuing competency [Board Rule 217.11(1)(G), (1)(H) & (1)(R)]. It is important for nurses to be aware of applicable policies and procedures related to these workplace issues.
- Nurses notify the appropriate supervisor when leaving a nursing assignment [Board Rule 217.11(1)(I)]. If the nurse is unable to provide care to a patient any longer due to threats or actual violence, a nurse must communicate with the supervisor regarding the inability to safely provide care to this patient before leaving the assignment, as adequate nursing care coverage must be obtained prior to leaving the assignment.
- Nurses know, recognize, and maintain professional boundaries of the nurse-client relationship [Board Rule 217.11(1)(J)]. The nurse has an obligation to establish, communicate and enforce professional boundaries, refraining from disparaging, violent, or unprofessional behavior in the presence of patients. Fostering healthy communications with the health care team is best for patient care.
- Nurses institute appropriate nursing interventions that might be required to stabilize a client’s condition and/or prevent complications, collaborating and consulting with the patient and members of the health care team in the interests of the patient’s care in an effort to promote a safe environment for all [Board Rule 217.11(1)(M) & (1)(P)]. When a patient could or has become violent, it important for the nurse to stabilize the patient to prevent further complications for the patient and the nurse. The nurse would need to collaborate with other health care providers to ensure the most appropriate care for the patient.
- Nurses must supervise the nursing care provided by others for whom the nurse is professionally responsible, ensuring the provision and maintenance of a safe patient care environment and make assignments to others that take into consideration client safety and that are commensurate with the educational preparation, experience, knowledge, and physical and emotional ability of the person to whom the assignments are made [Board Rule 217.11 (1)(U) & (1)(S)]. When making assignments that involve potentially violent patients, it is important to take into consideration the safety, knowledge, skills, and abilities of the nurse to whom the assignments are made.
- Nurses accept only those nursing assignments that take into consideration client safety and that are commensurate with the nurse’s educational preparation, experience, knowledge, and physical and emotional ability; and provide, without discrimination, nursing services regardless of the age, disability, economic status, gender, national origin, race, religion, health problems, or sexual orientation of the client served [Board Rule 217.11 (1)(T) & (1)(L)]. Nurses must take into consideration any preconceived notions they may have about a patient that has the potential to, or has already become, violent. A nurse would need to determine if he/she has received the appropriate education and training to have the knowledge, skills, and abilities to provide safe care to a potentially violent patient. Collaboration must occur with the healthcare team to ensure safe care is provided to the patient.
Behaviors associated with workplace violence compromise the safety of the patient and the health care team. Nurse leaders must assess their organizations for workplace violence and implement policies that support a framework to systematically reduce workplace violence.6 It is a shared responsibility among nurses and employers to create an environment in which both nurses and patients feel safe.
References
1American Nurses Association (2015). Position Statement: Incivility, Bullying, and Workplace Violence. Retrieved from https://www.nursingworld.org/~49d6e3/globalassets/practiceandpolicy/nursing-excellence/incivility-bullying-and-workplace-violence--ana-position-statement.pdf
2U.S. Department of Labor Occupational Safety and Health Administration (2017). Workplace Violence. Retrieved from https://www.osha.gov/SLTC/workplaceviolence/
3U.S. Department of Labor Occupational Safety and Health Administration (2016). Guidelines for preventing workplace violence for healthcare and social service workers. Retrieved from https://www.osha.gov/Publications/osha3148.pdf
4Texas Department of State Health Services Texas Center for Nursing Workforce Studies (2016). Workplace Violence Against Nurses in Texas. Retrieved from www.dshs.texas.gov/legislative/2016-Reports/DSHS-Report-HB2696.pdf
5Texas Board of Nursing. (2013). When do nurses have a duty to report confidential health information. Texas Board of Nursing Bulletin, 44(2), 5-6.
6The American organization of Nurse Executives and the Emergency Nurses Association (2015). Toolkit for Mitigating Violence in the Workplace. Retrieved from http://www.aone.org/resources/final_toolkit.pdf
(Adopted: 01/2018)
(Reviewed: 01/2019; 01/2020; 01/2021)
Return to top |
| |